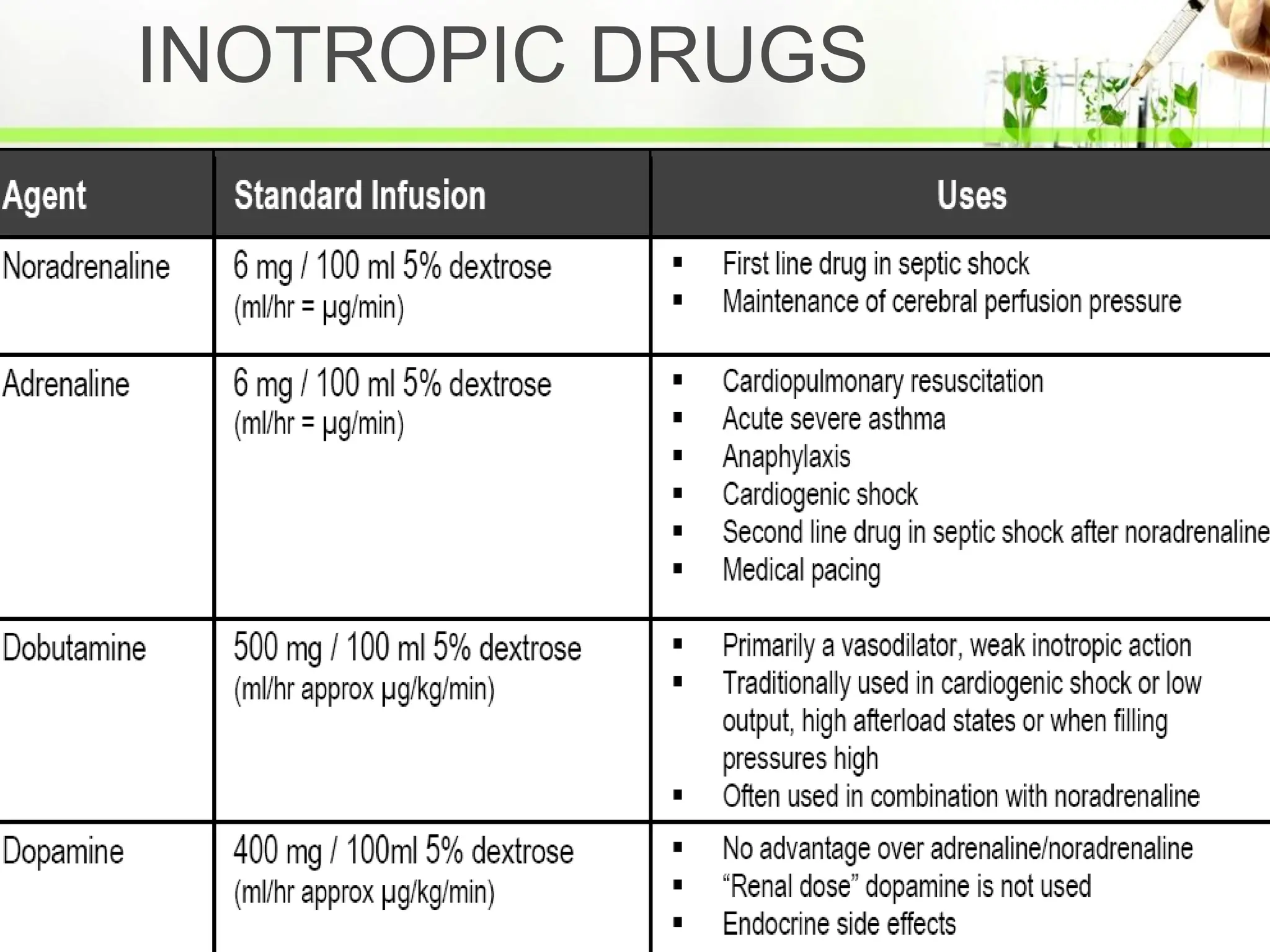
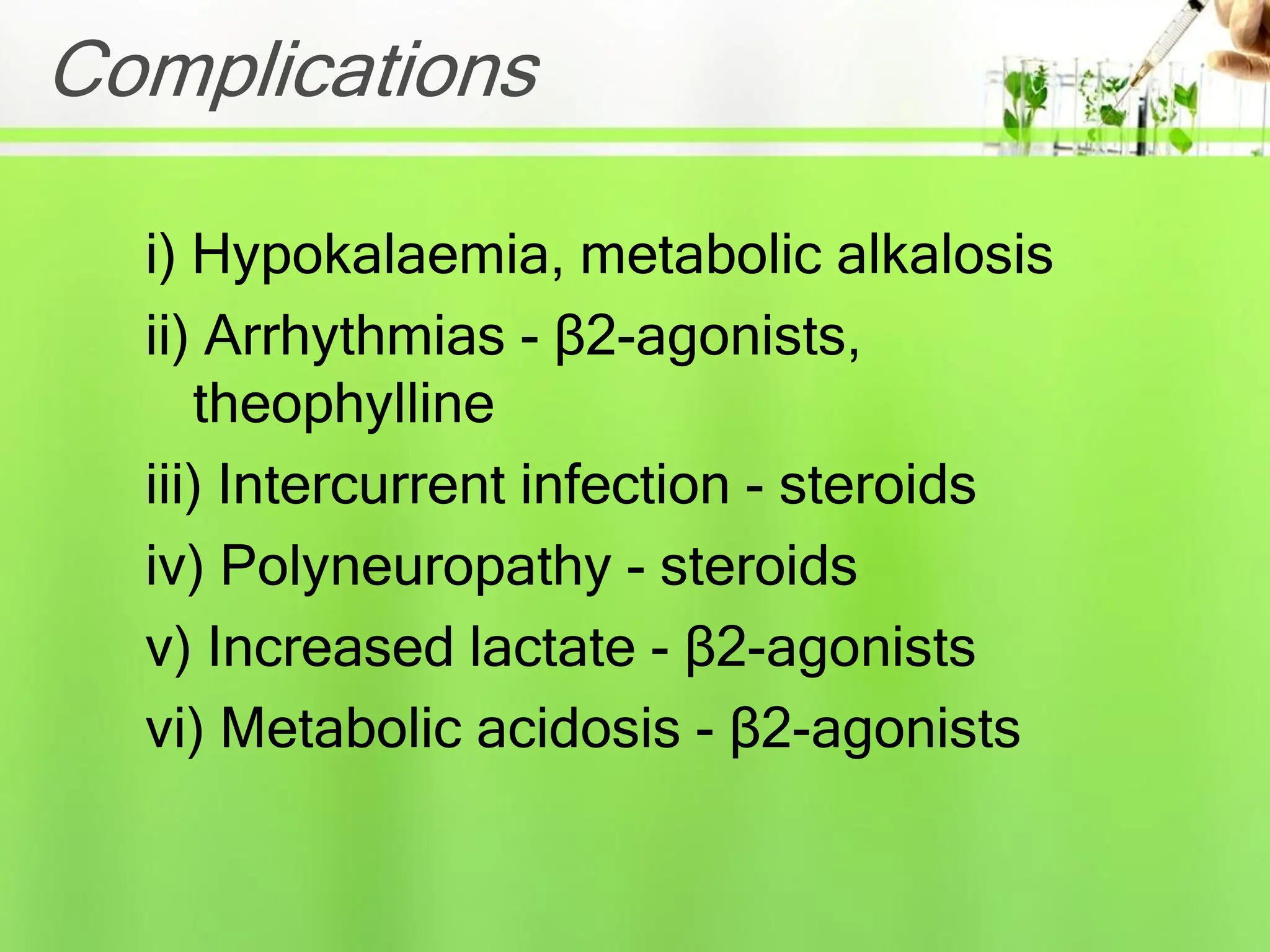
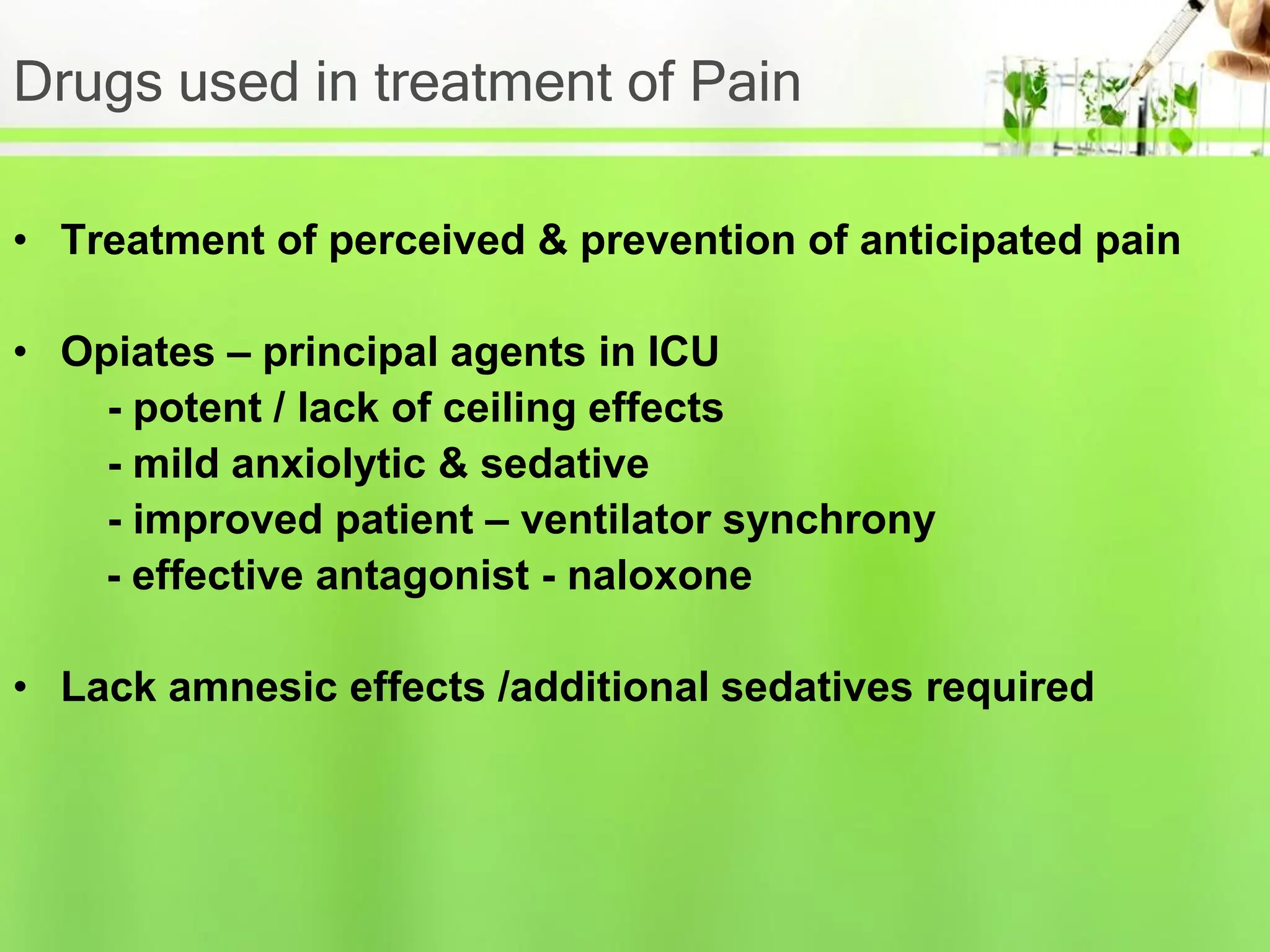
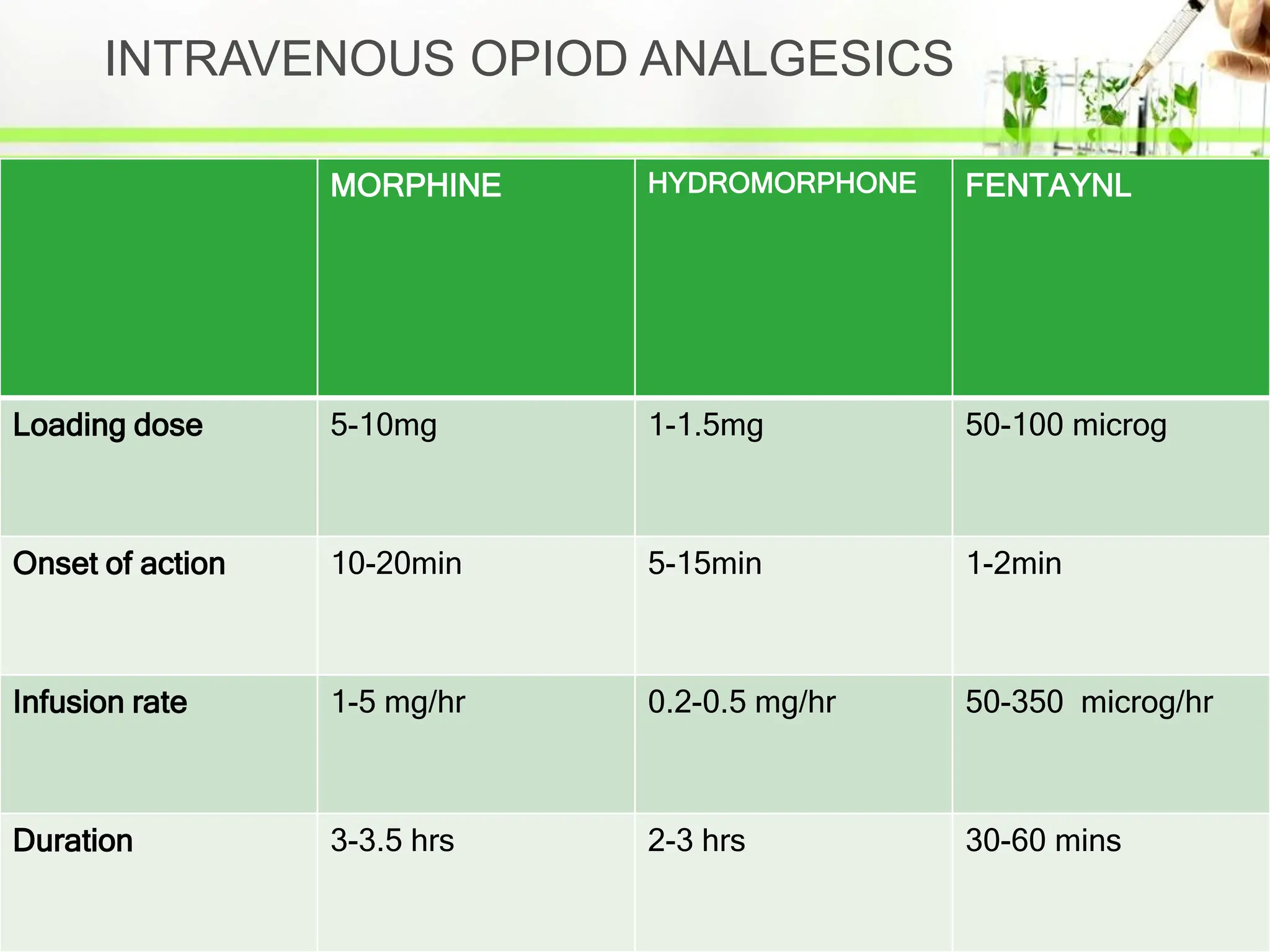
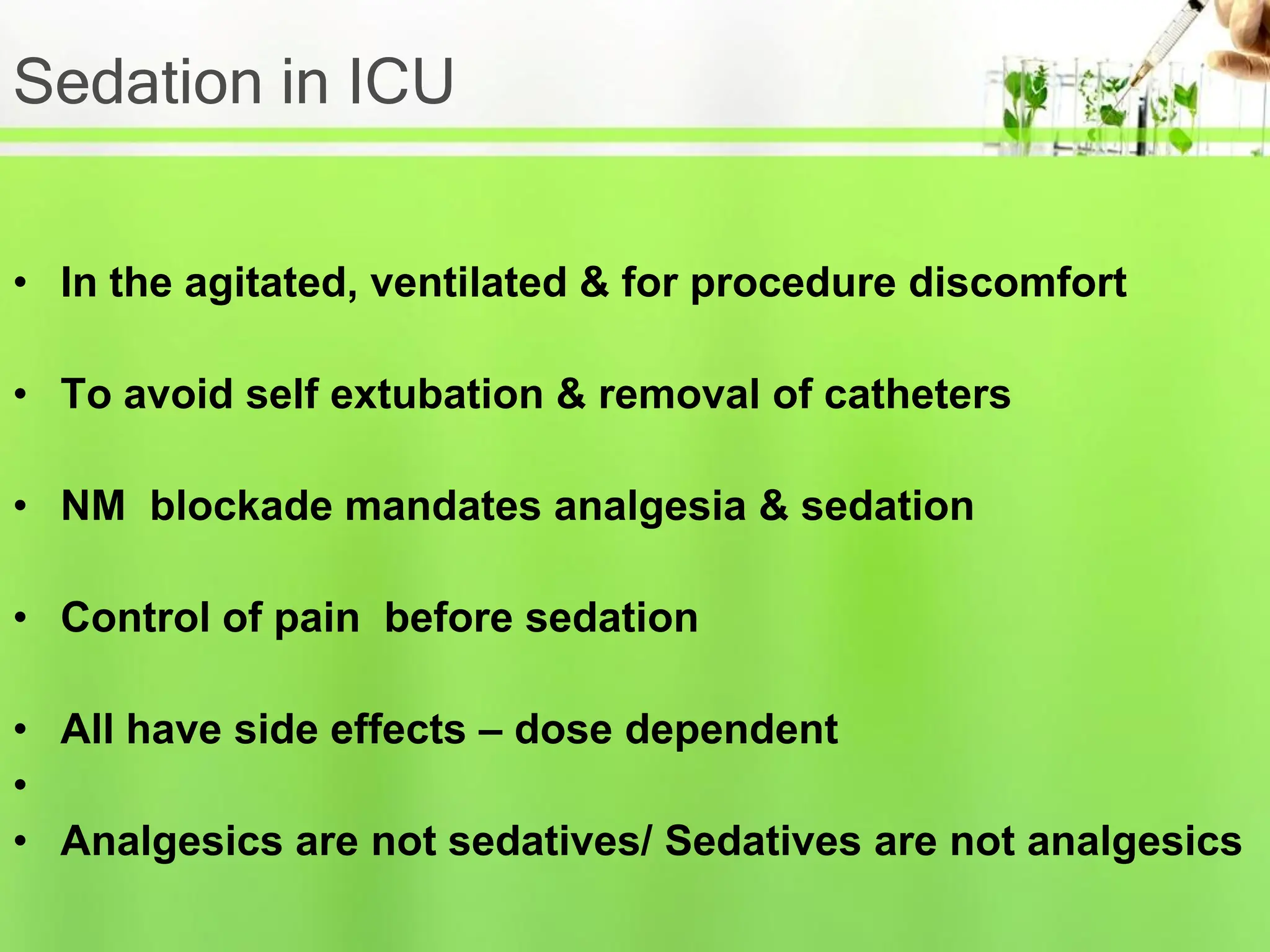
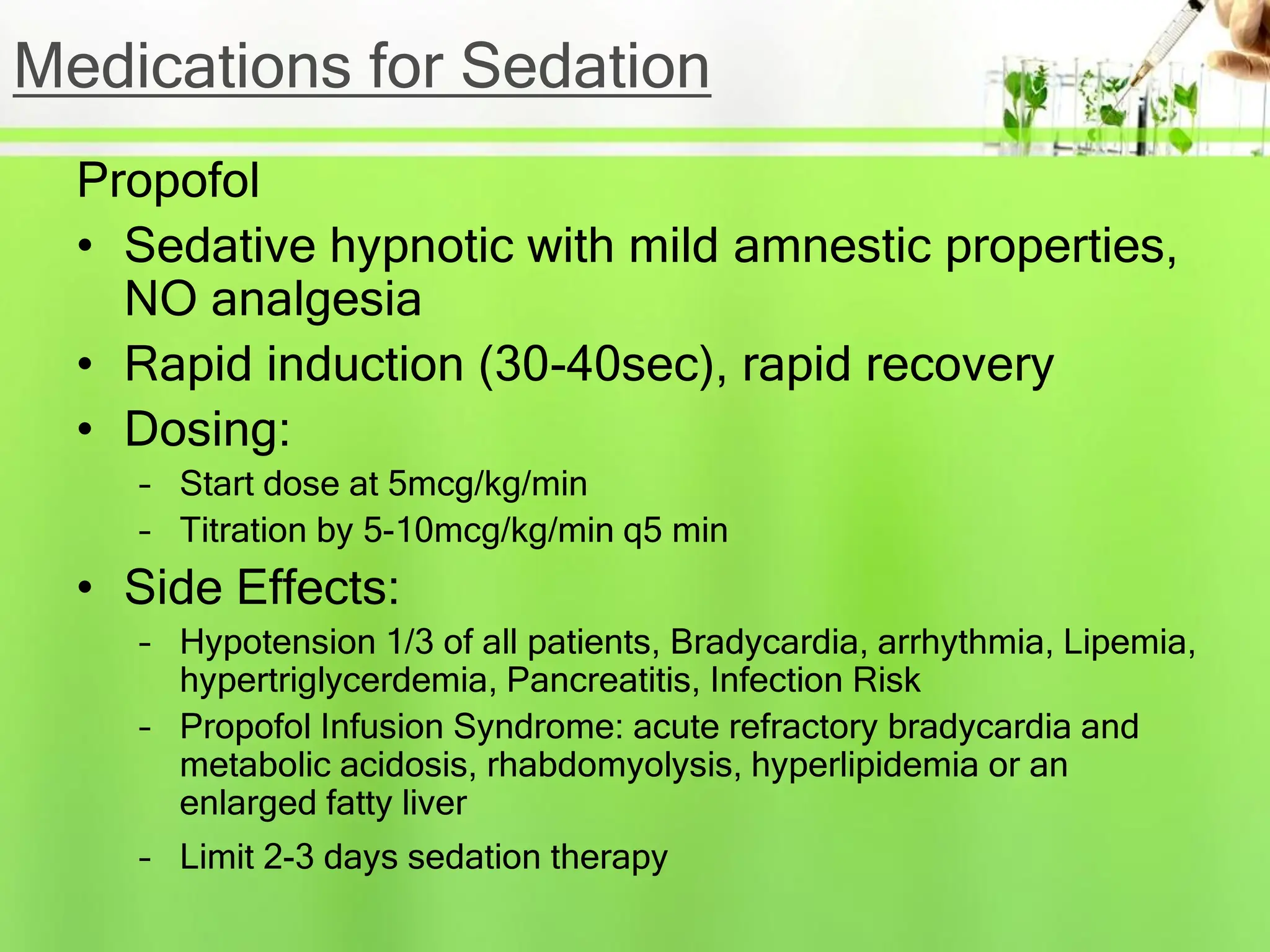
The document outlines the policy and guidelines for drug use in ICU, emphasizing the importance of a thorough drug history for patients and adherence to unit protocols. It covers various drug categories, including cardiovascular and respiratory medications, as well as sedation, analgesia, and anticoagulation, while highlighting monitoring, potential interactions, and complications. The document also stresses the need for optimal dosing and the consideration of cost-effectiveness in drug selection for critically ill patients.