This document discusses the radiological presentation and staging of musculoskeletal tumors. It covers:
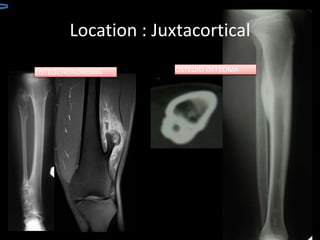
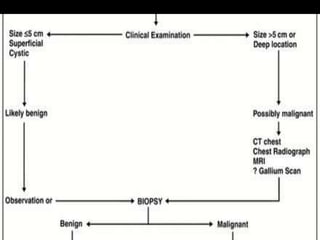
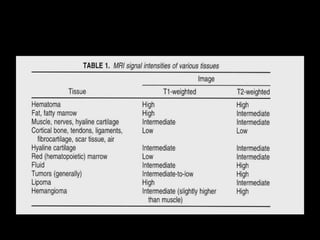
1. The importance of plain radiographs and MRI in assessing bone and soft tissue tumors.
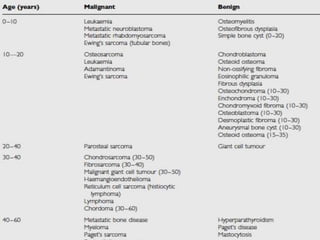
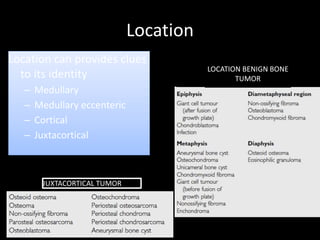
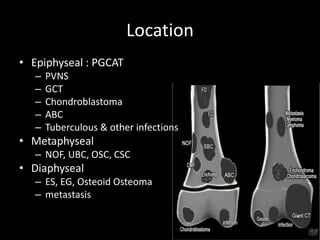
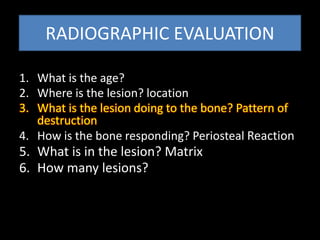
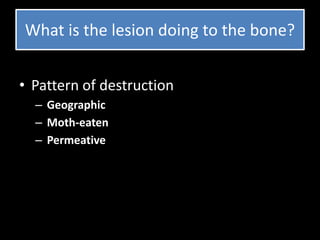
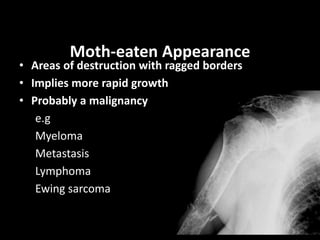
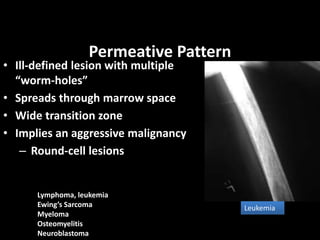
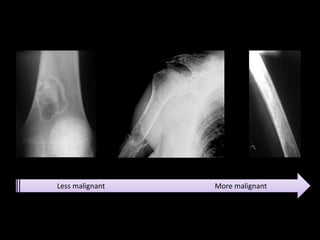
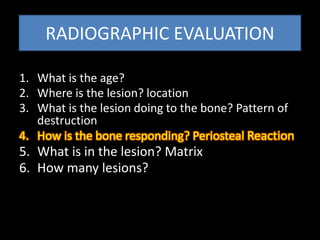
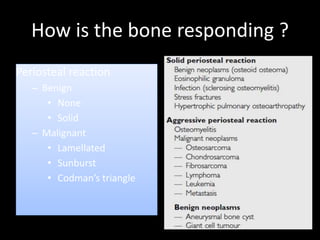
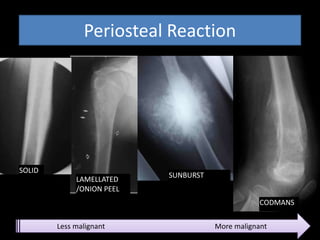
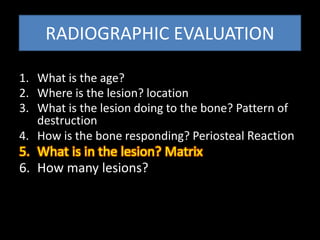
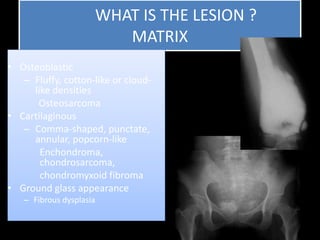
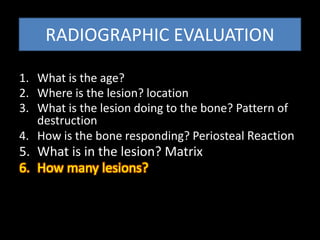
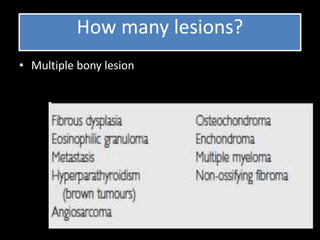
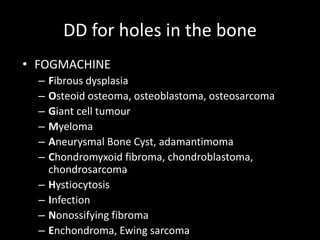
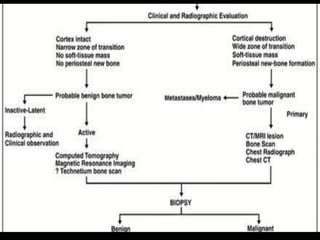
2. A 6-point system for radiographic evaluation of bone lesions including location, pattern of bone destruction, periosteal reaction, lesion matrix, number of lesions, and age.
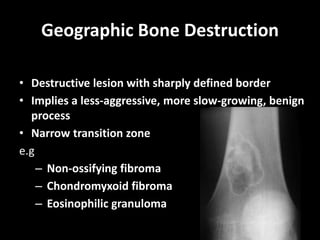
3. Examples of benign and malignant patterns of bone destruction, periosteal reactions, and lesion matrices.
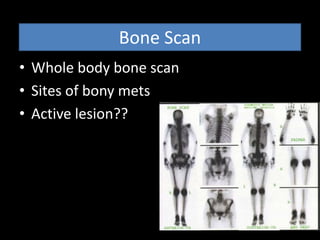
4. Staging studies like CT, MRI, bone scan and chest CT to determine tumor type, prognosis, treatment and presence of metastases.
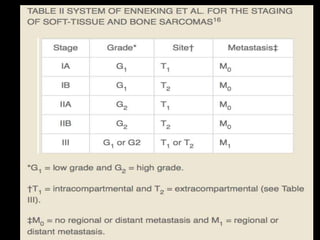
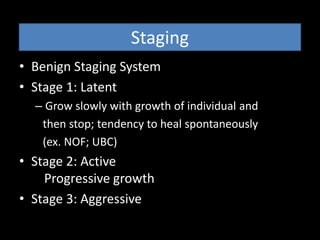
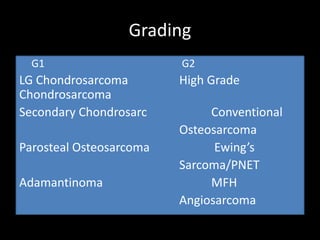
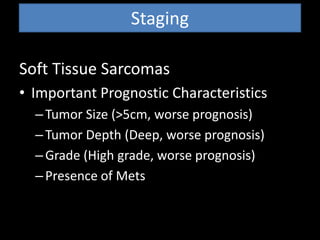
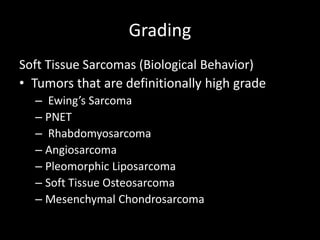
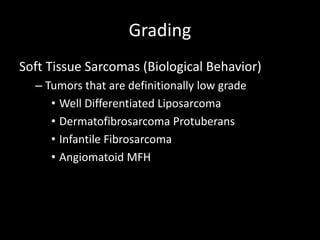
5. Staging systems for benign and malignant bone tumors as well as soft