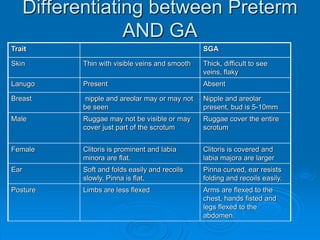
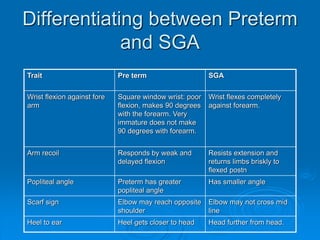
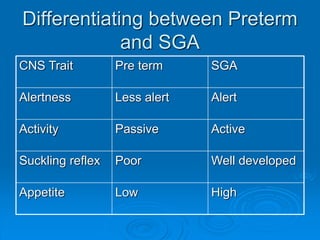
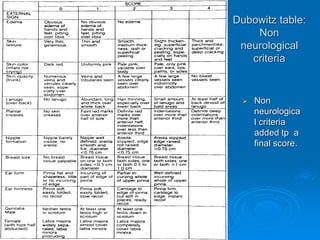
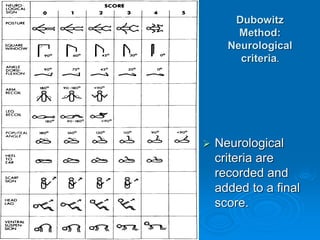
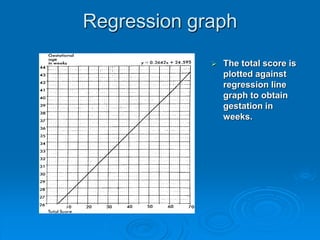
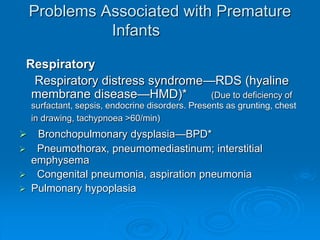
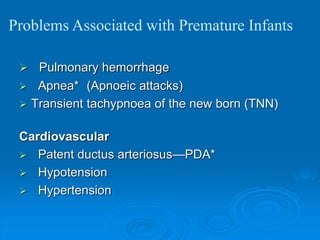
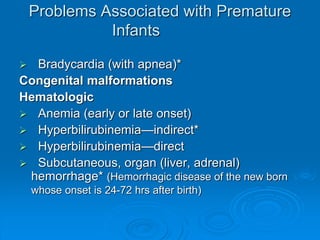
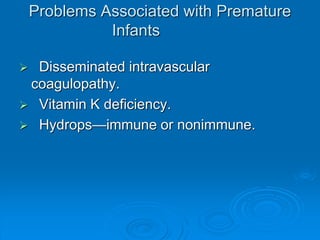
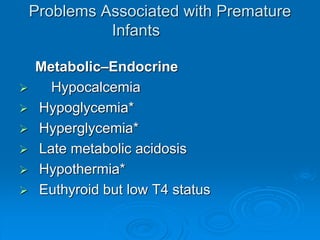
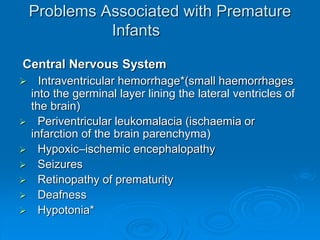
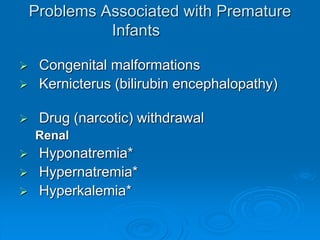
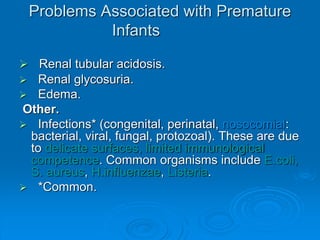
This document defines prematurity and related terms like low birth weight (LBW), small for gestational age (SGA), very low birth weight (VLBW), and extremely low birth weight (ELBW). It discusses the public health importance of prematurity, describing the high rates of prematurity globally and associated increased mortality. The document outlines maternal and fetal risk factors for prematurity and methods for differentiating preterm and SGA infants. It also provides extensive details on potential health complications in preterm infants and recommendations for management and prevention.