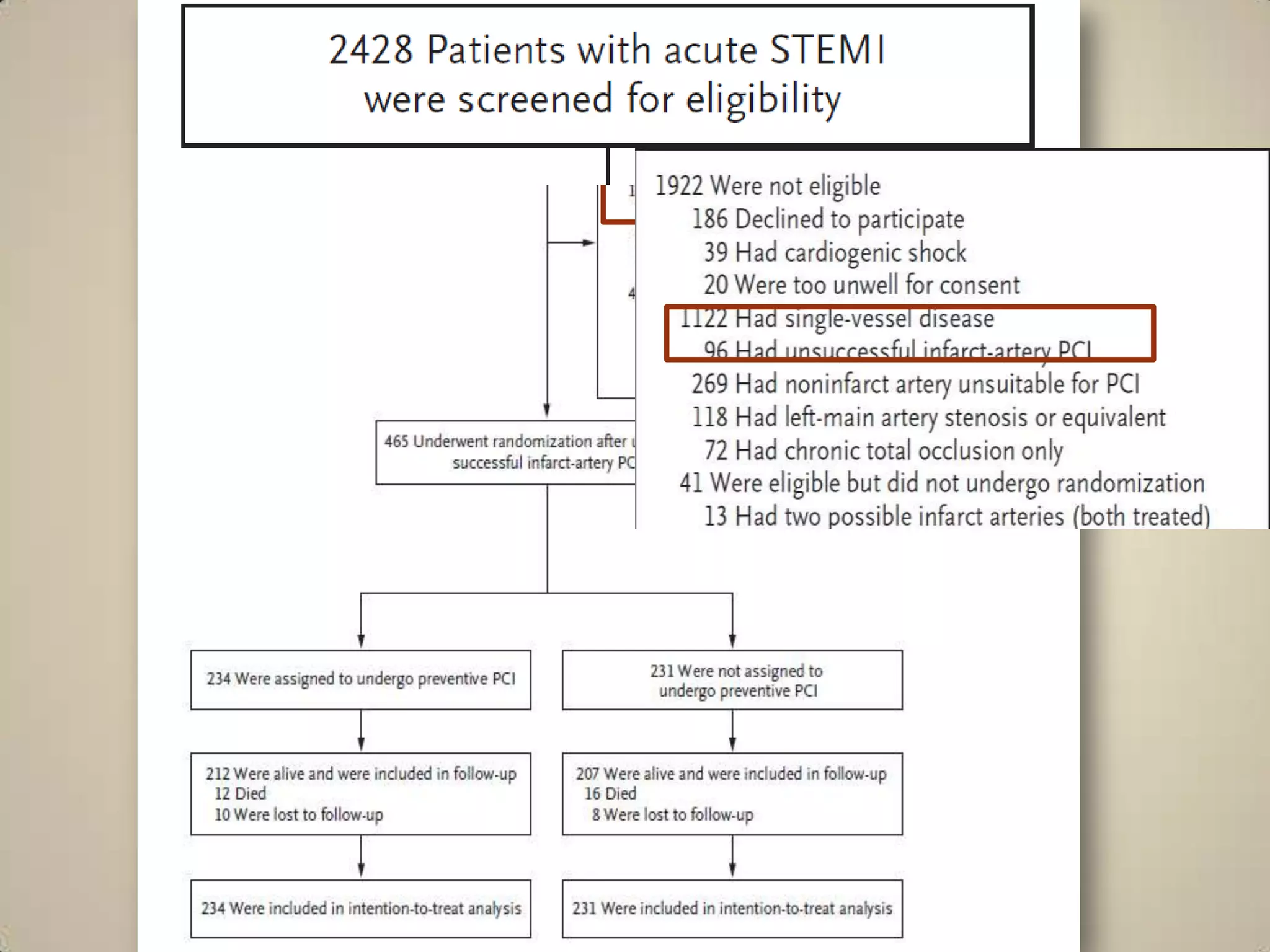
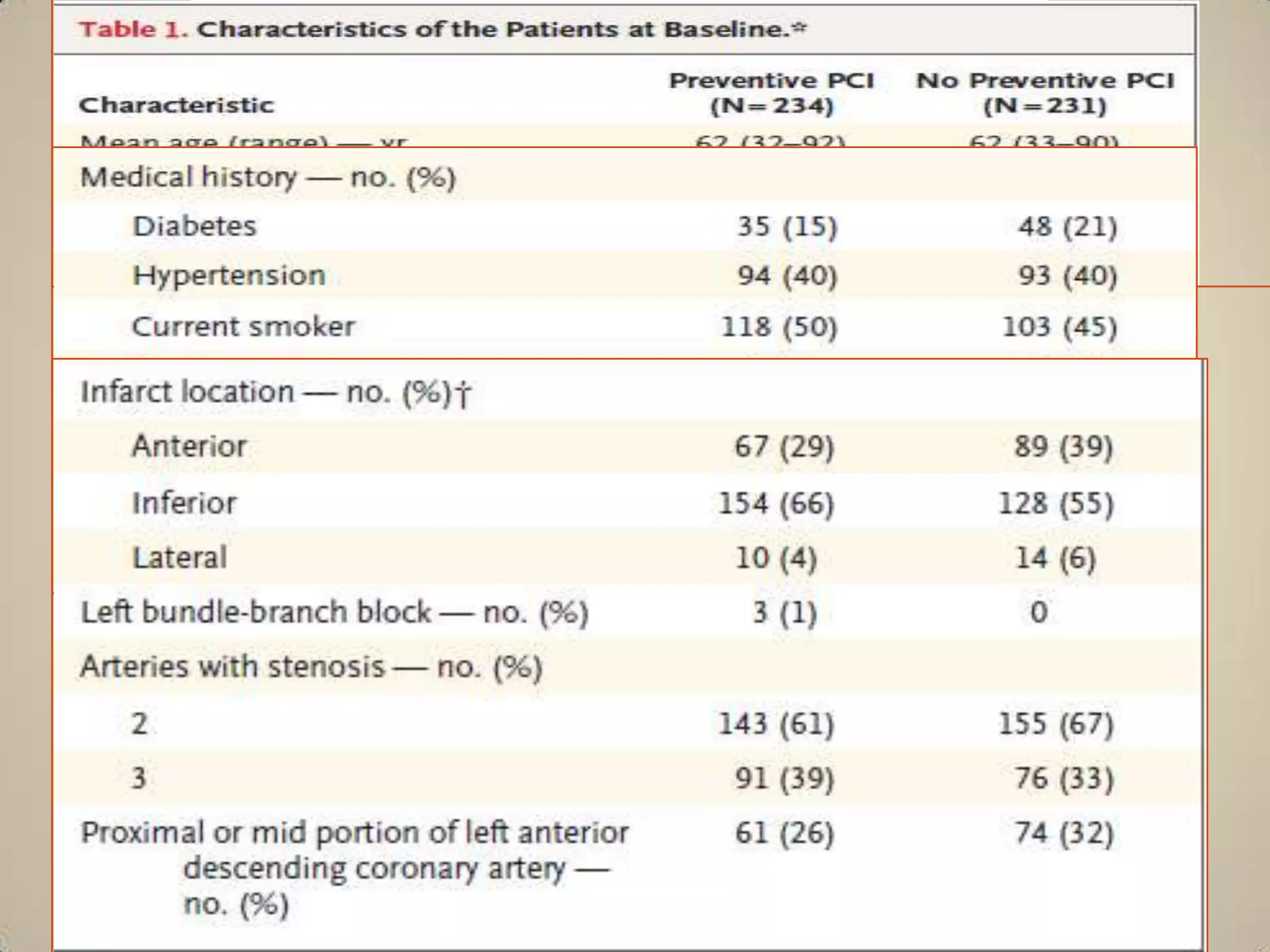
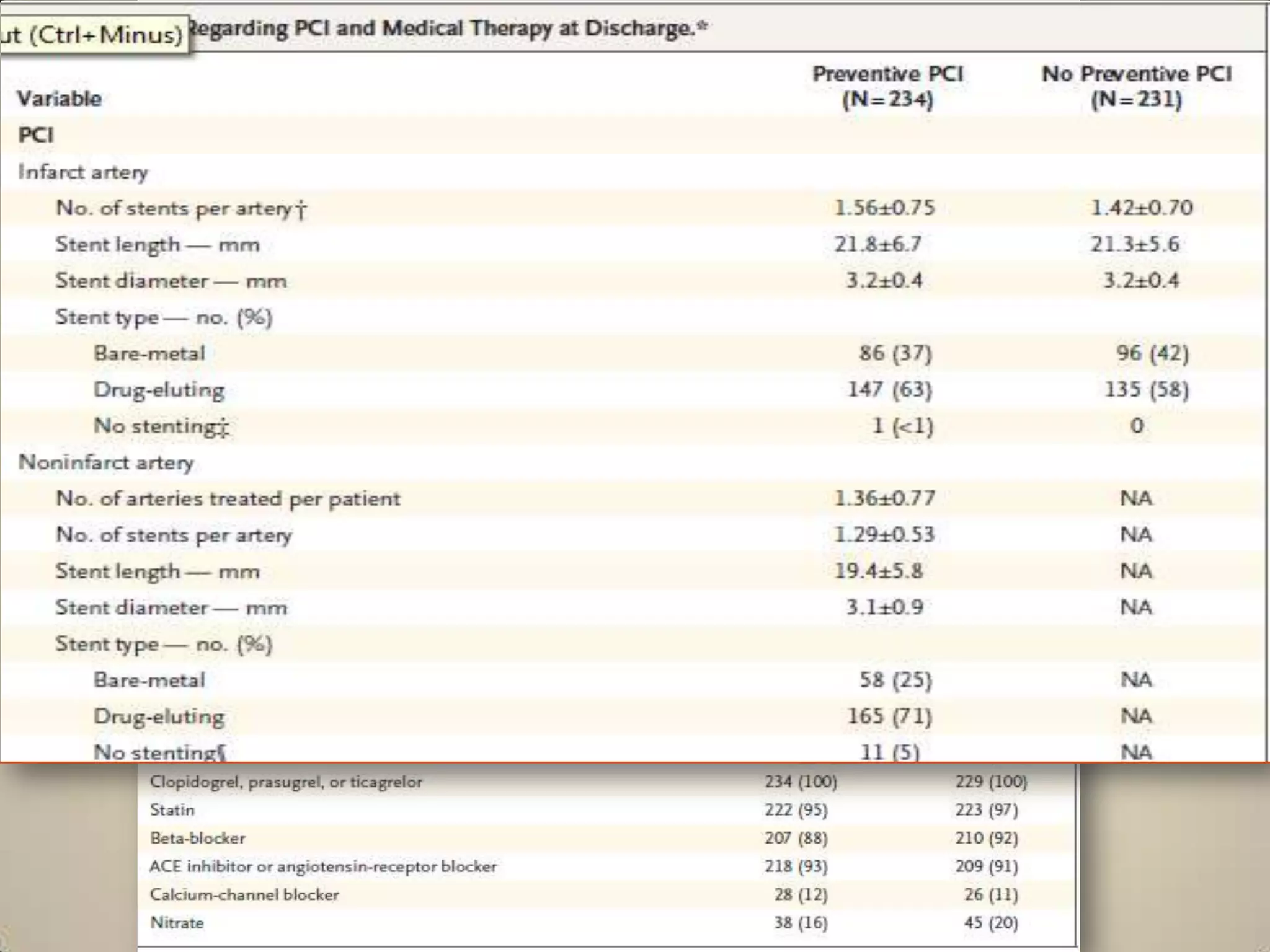
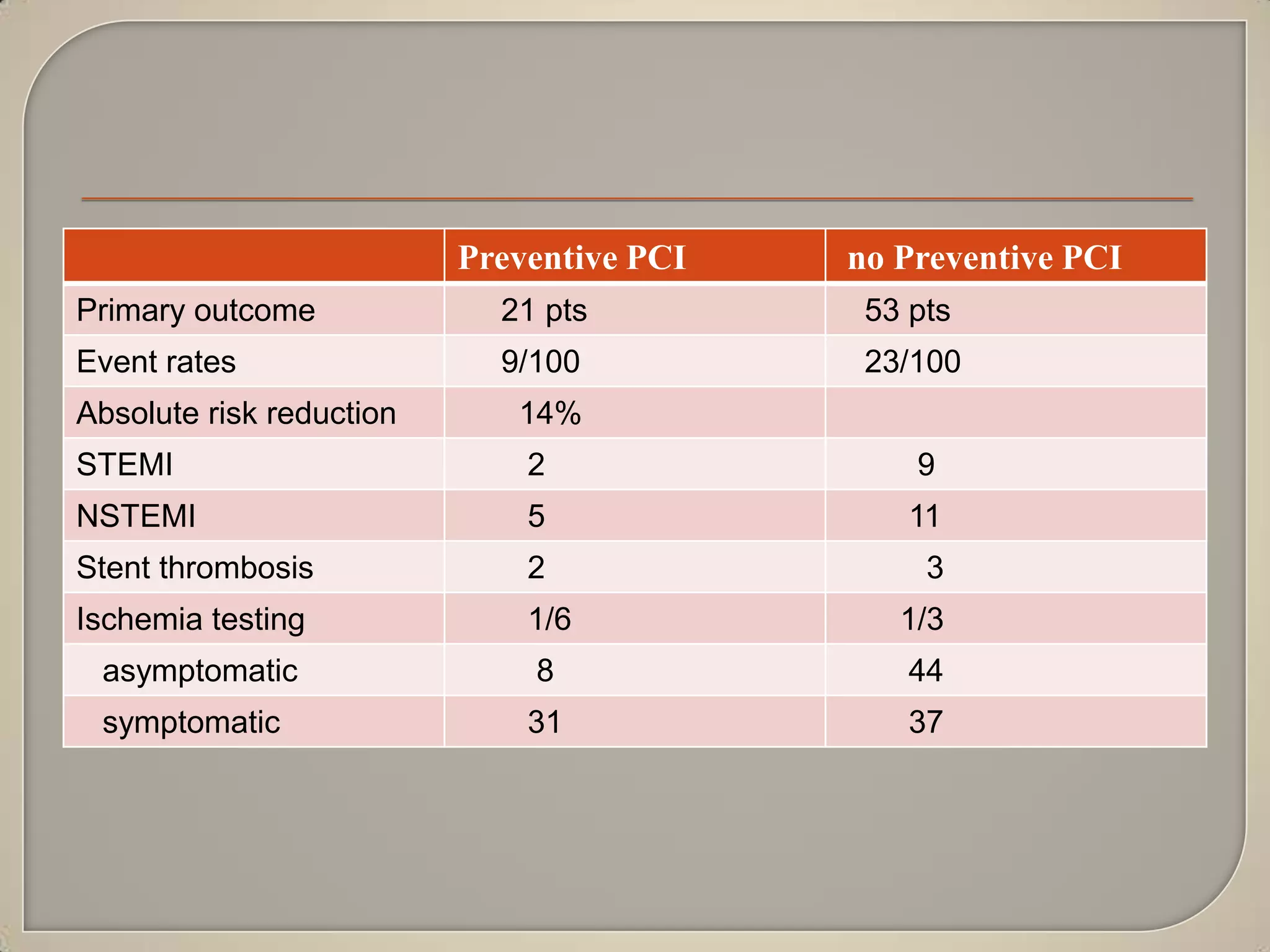
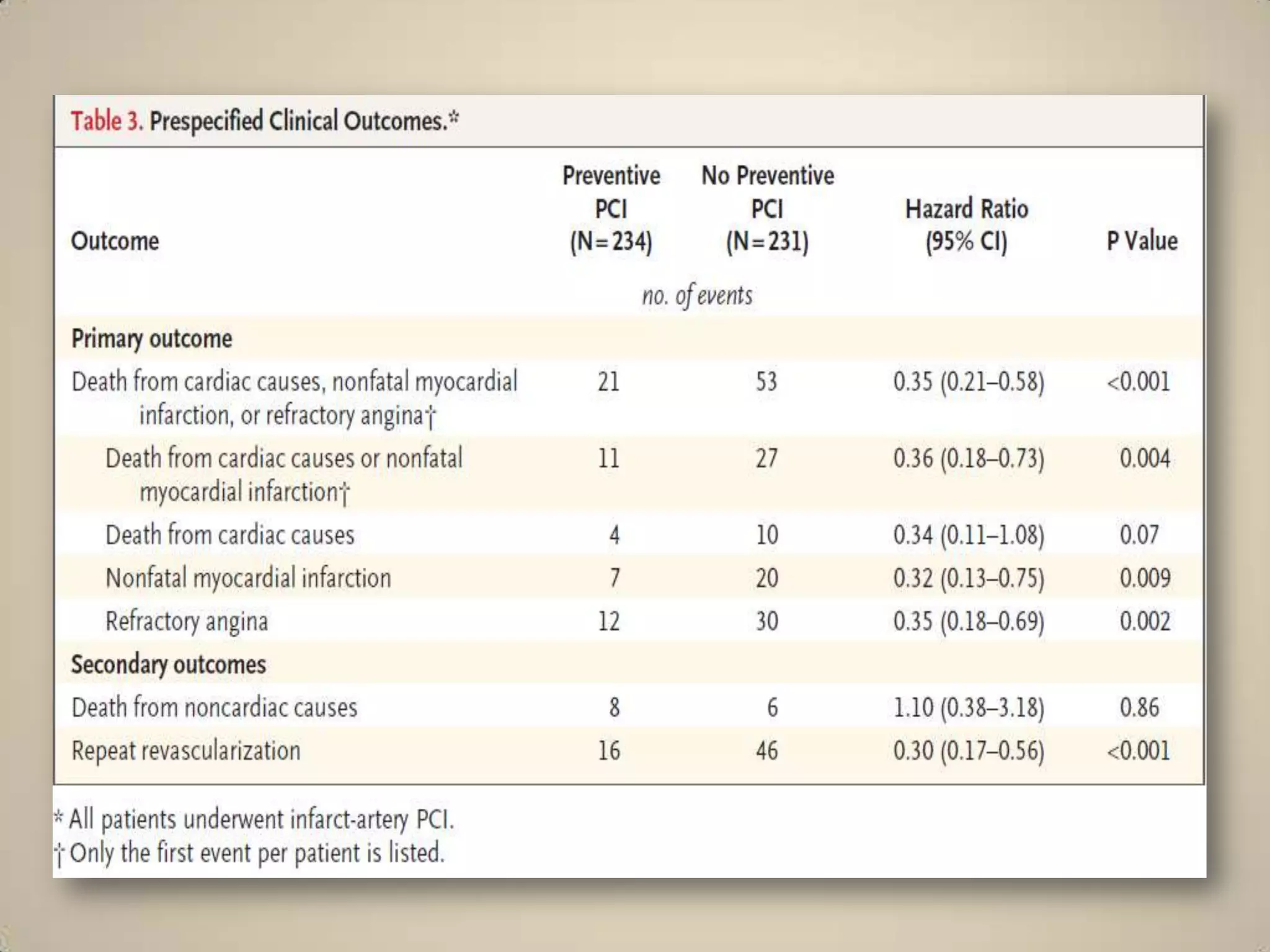
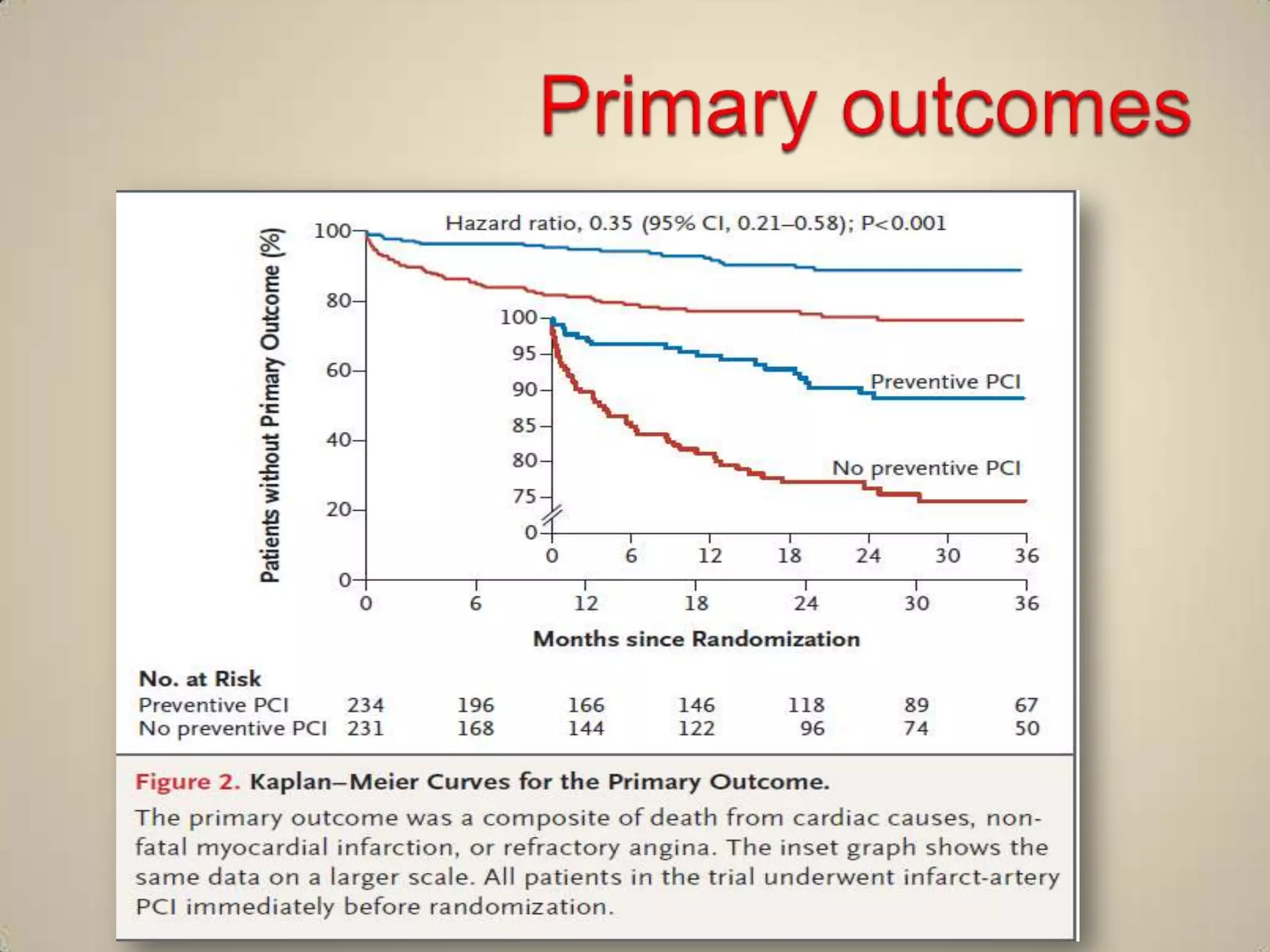
A randomized study assigned 465 patients undergoing emergency PCI for acute STEMI to either preventive PCI of stenoses in non-infarct arteries or PCI of the infarct artery only. At a mean follow up of 23 months, the preventive PCI group had lower rates of the primary composite outcome of death from cardiac causes, non-fatal heart attack, or refractory angina (9% vs 23%). Preventive PCI also reduced the risk of subsequent cardiovascular events within the first 6 months after the procedure. Procedure times and contrast usage were increased with preventive PCI, but complication rates were similar between the groups.