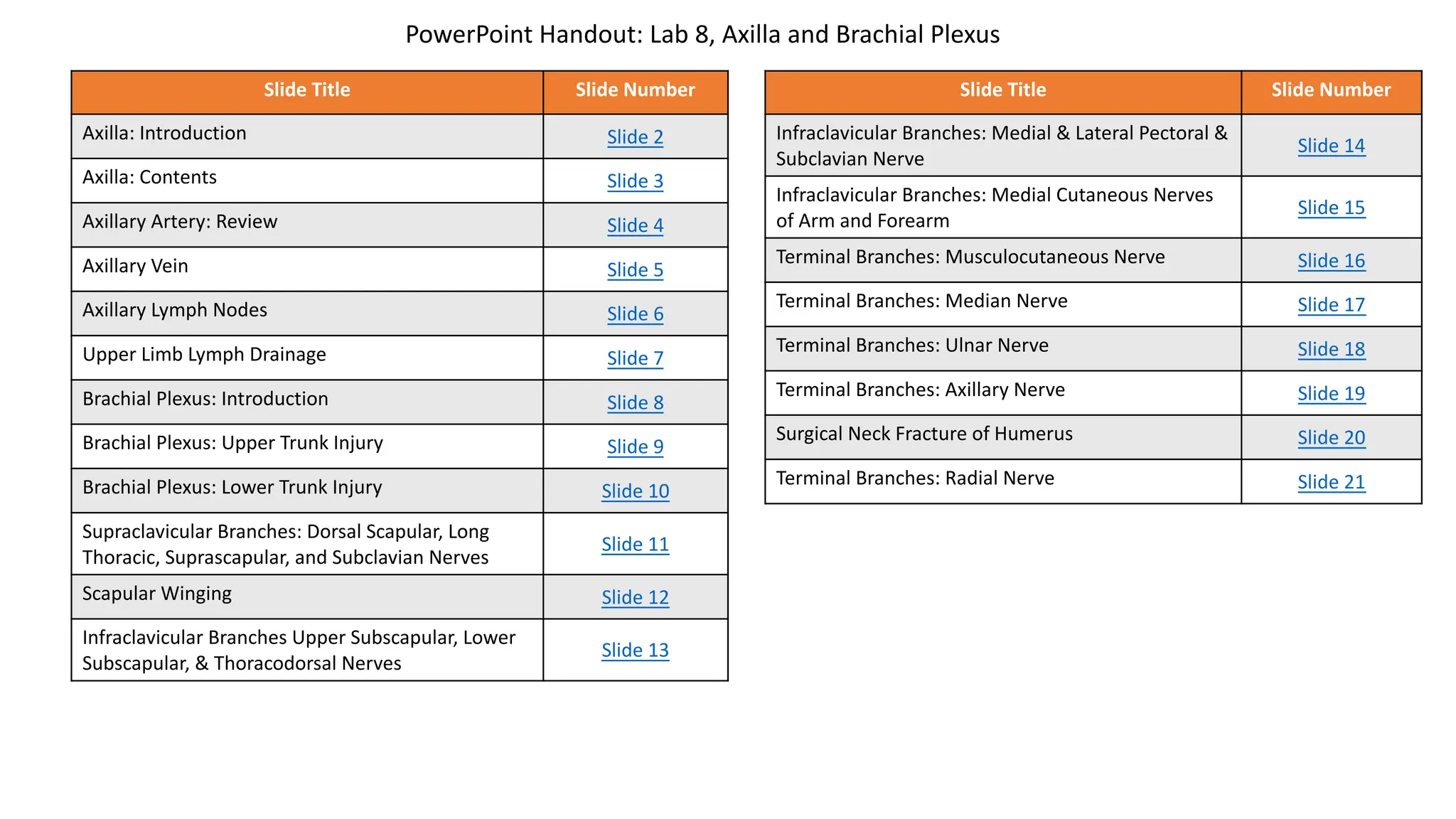
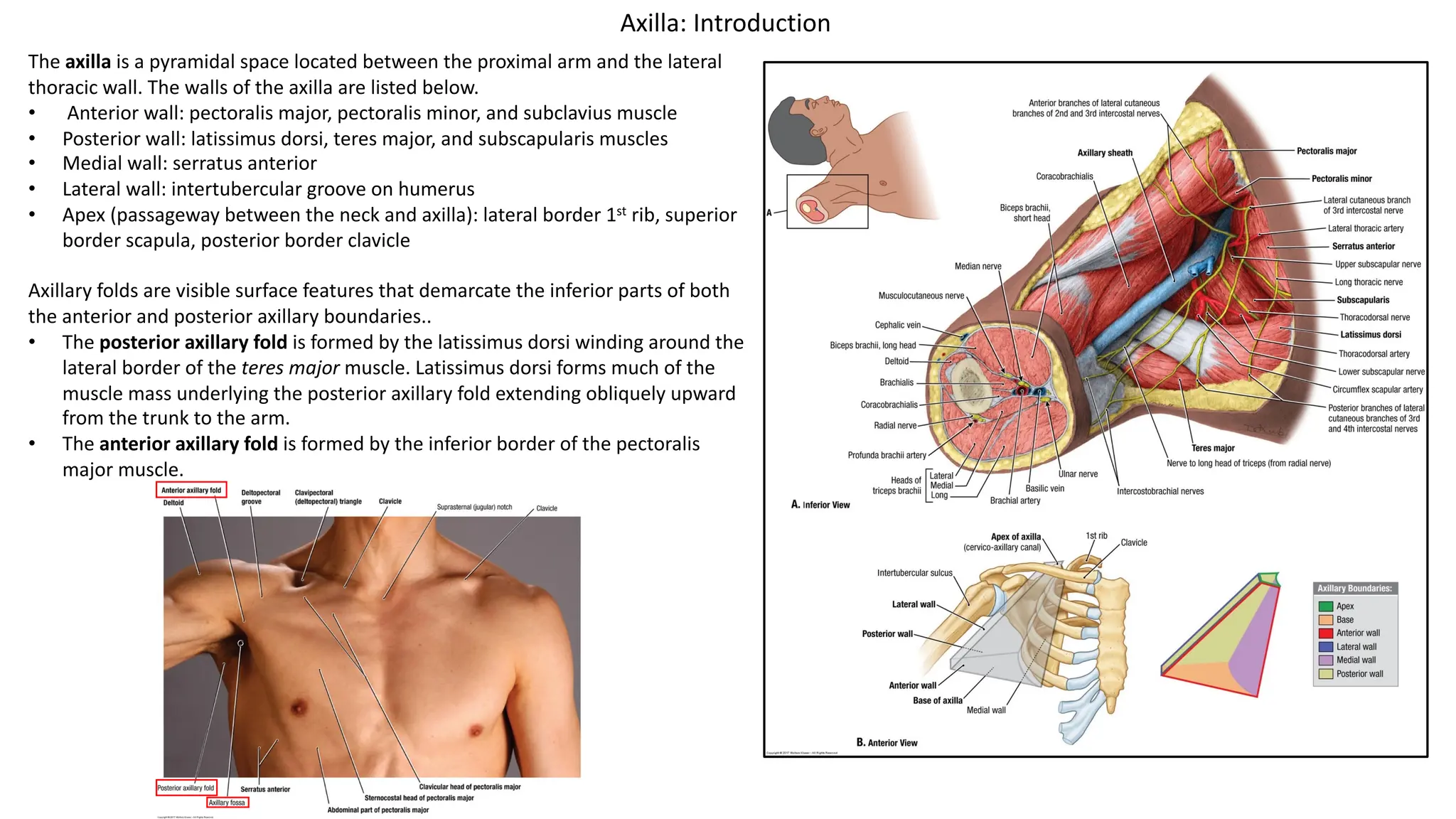
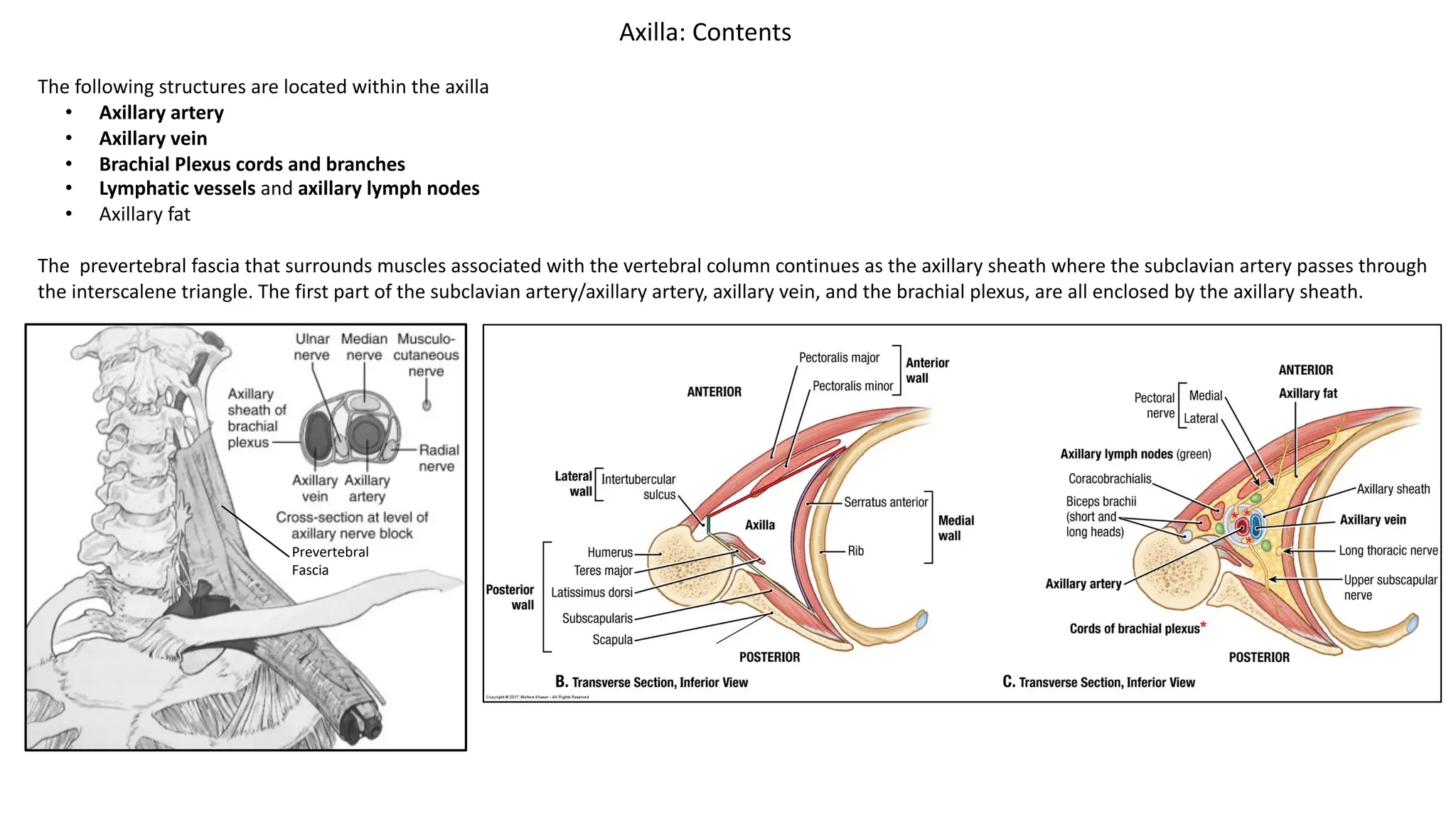
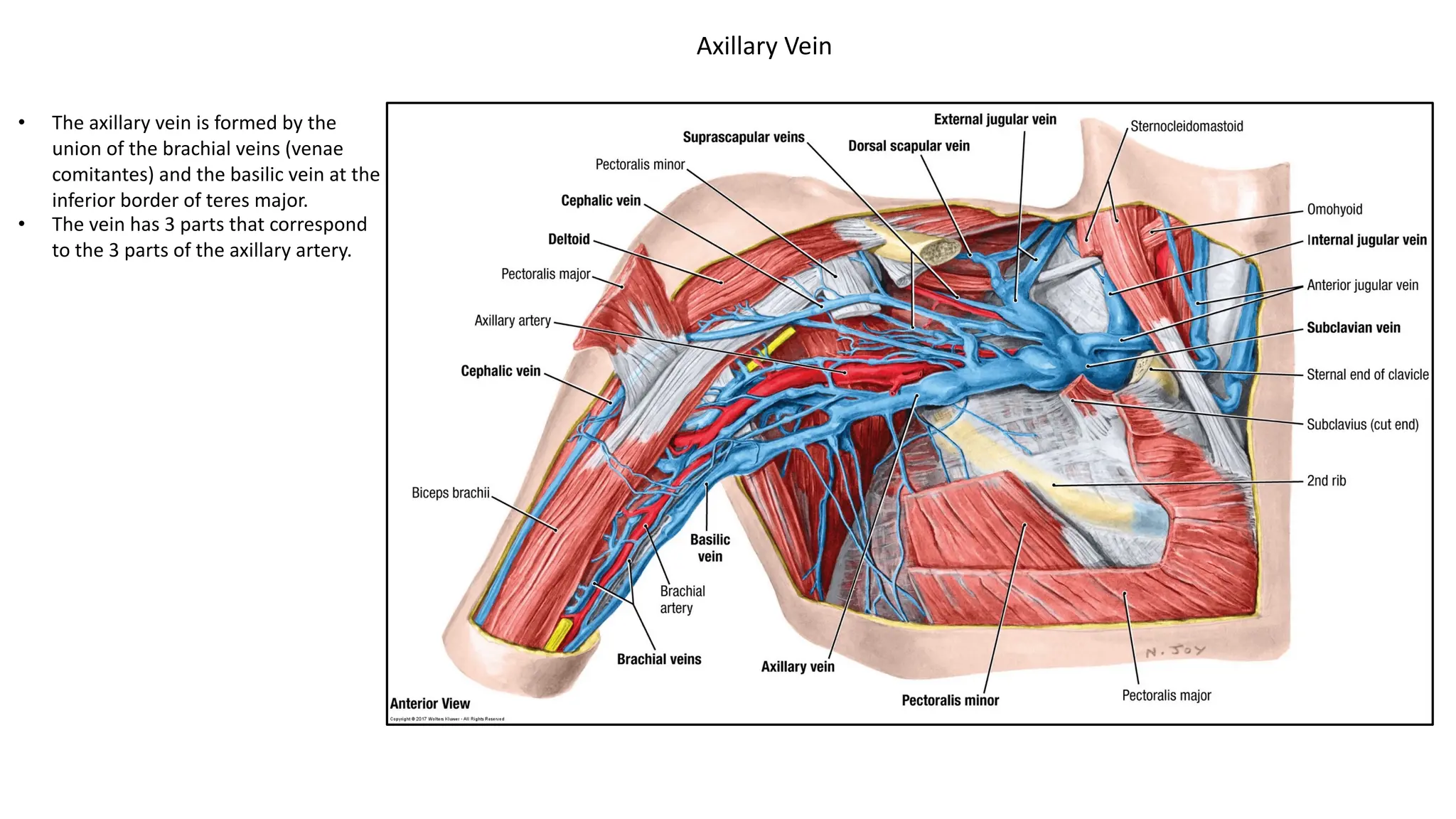
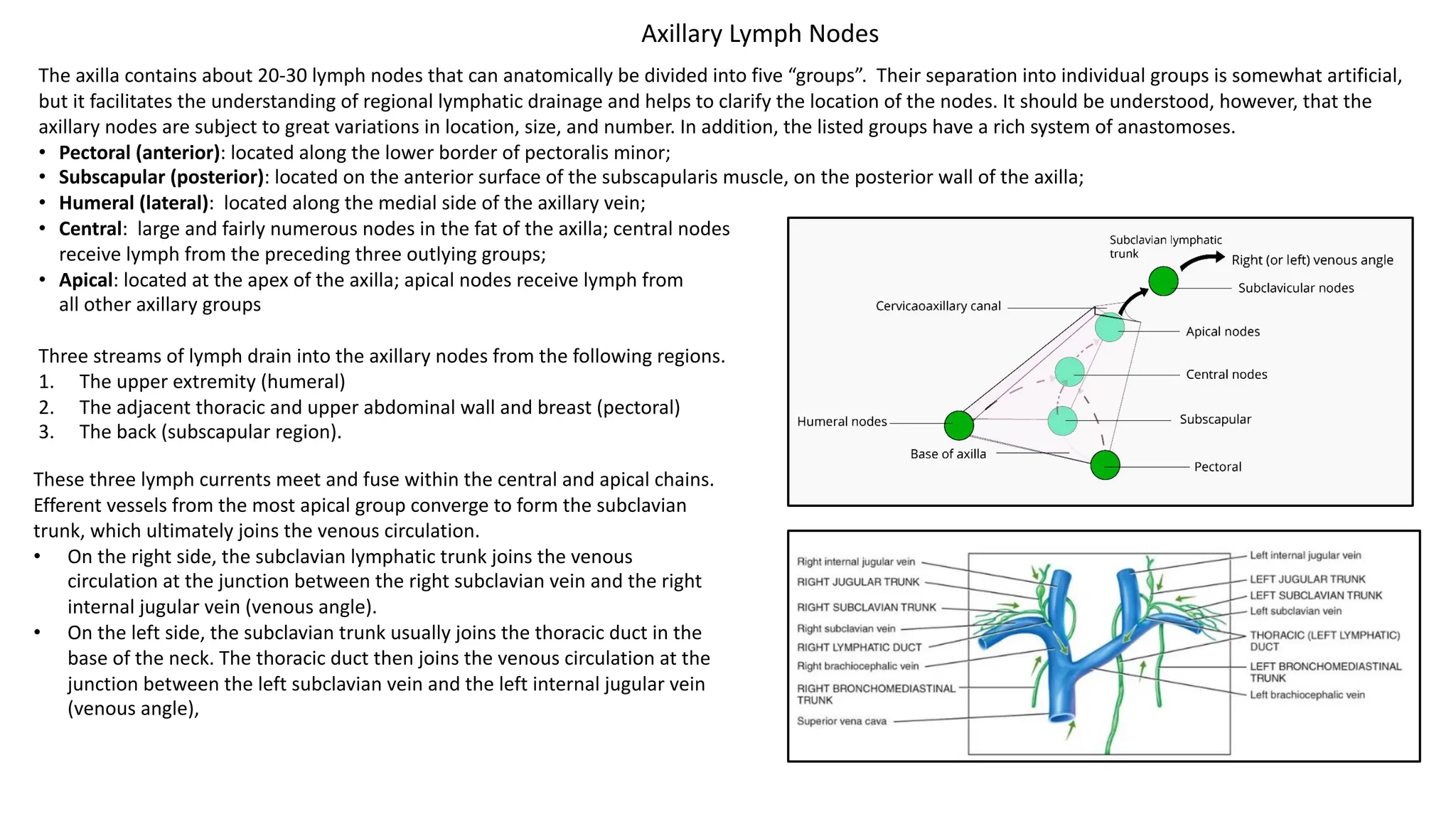
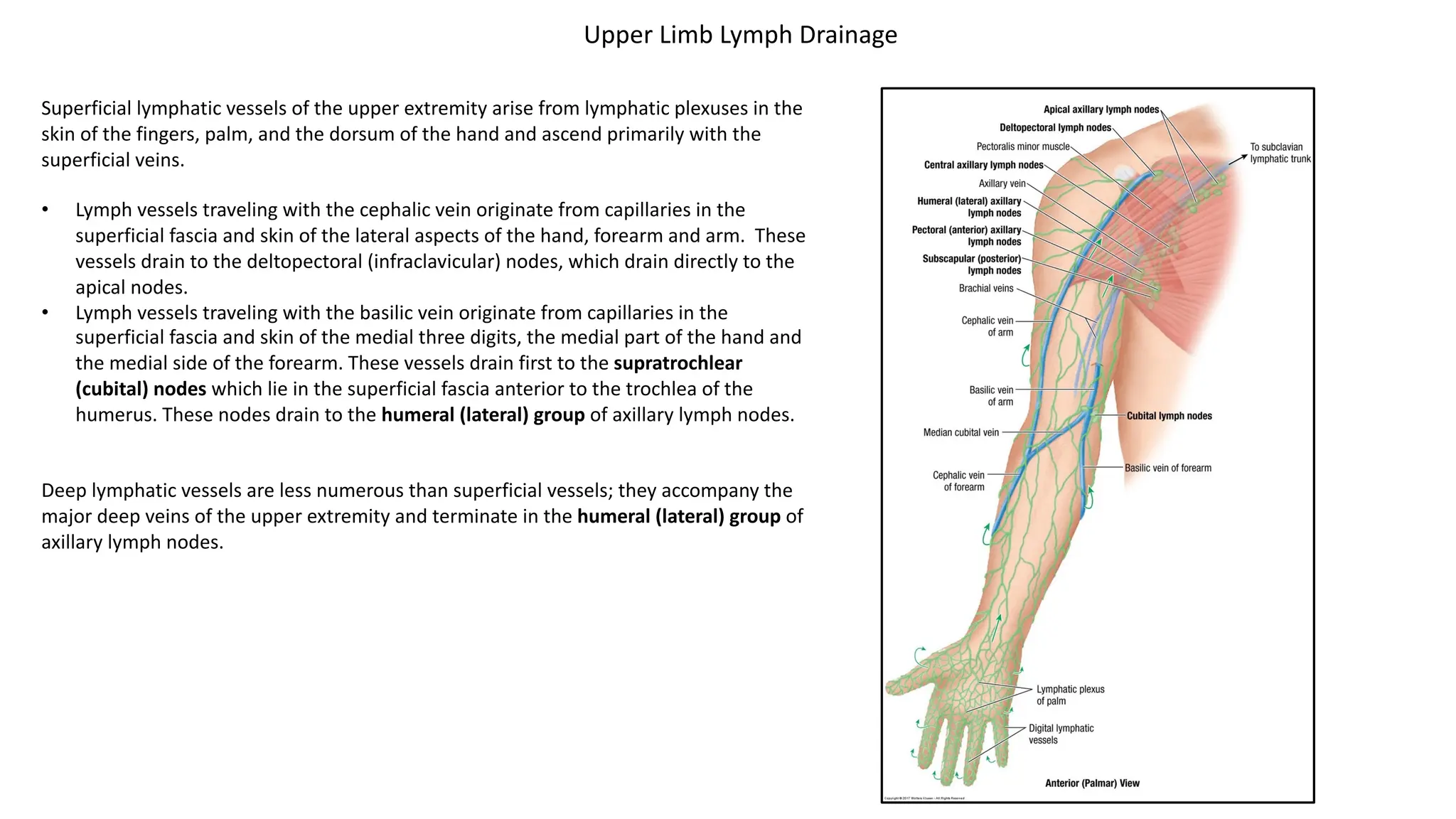
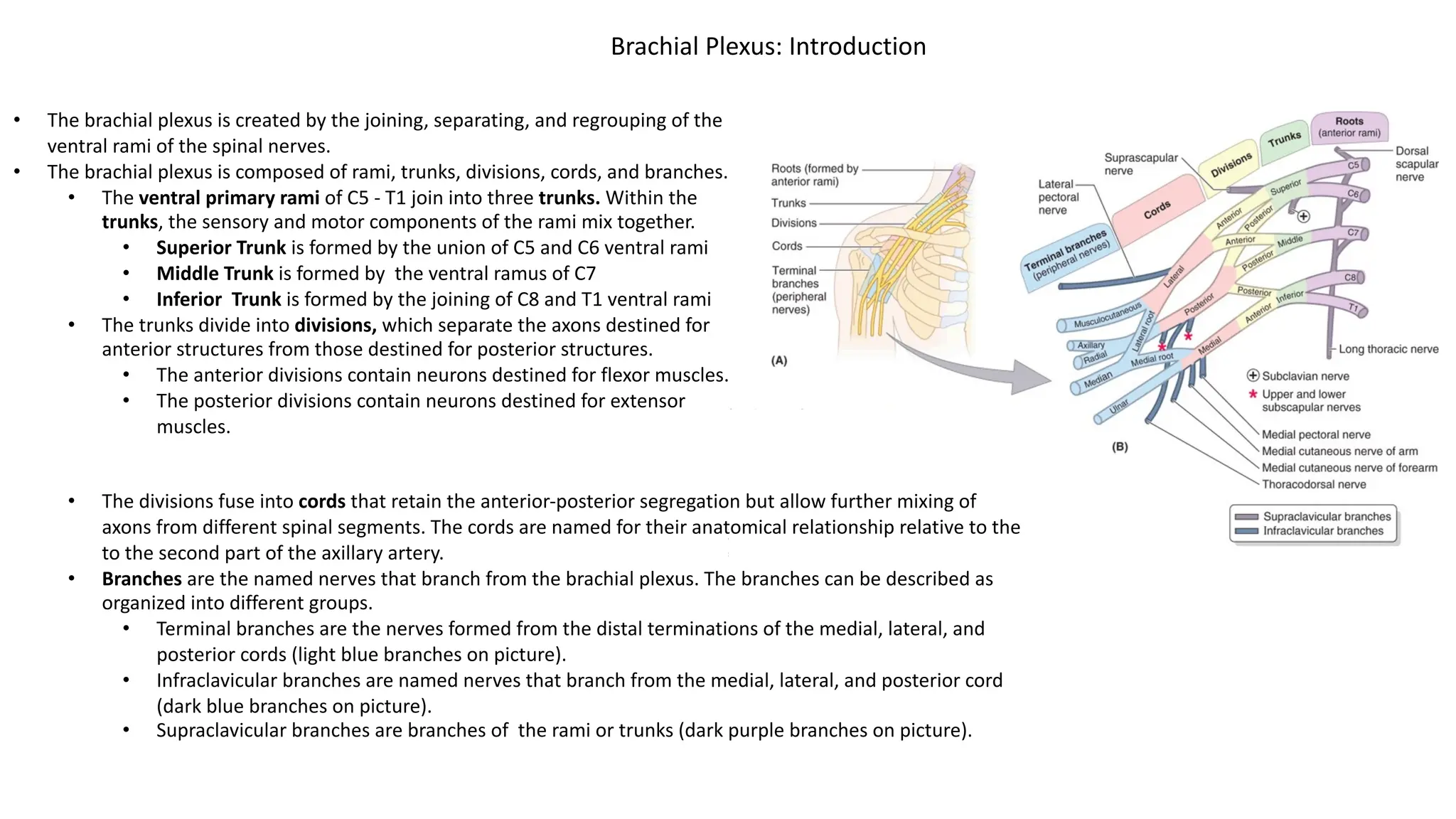
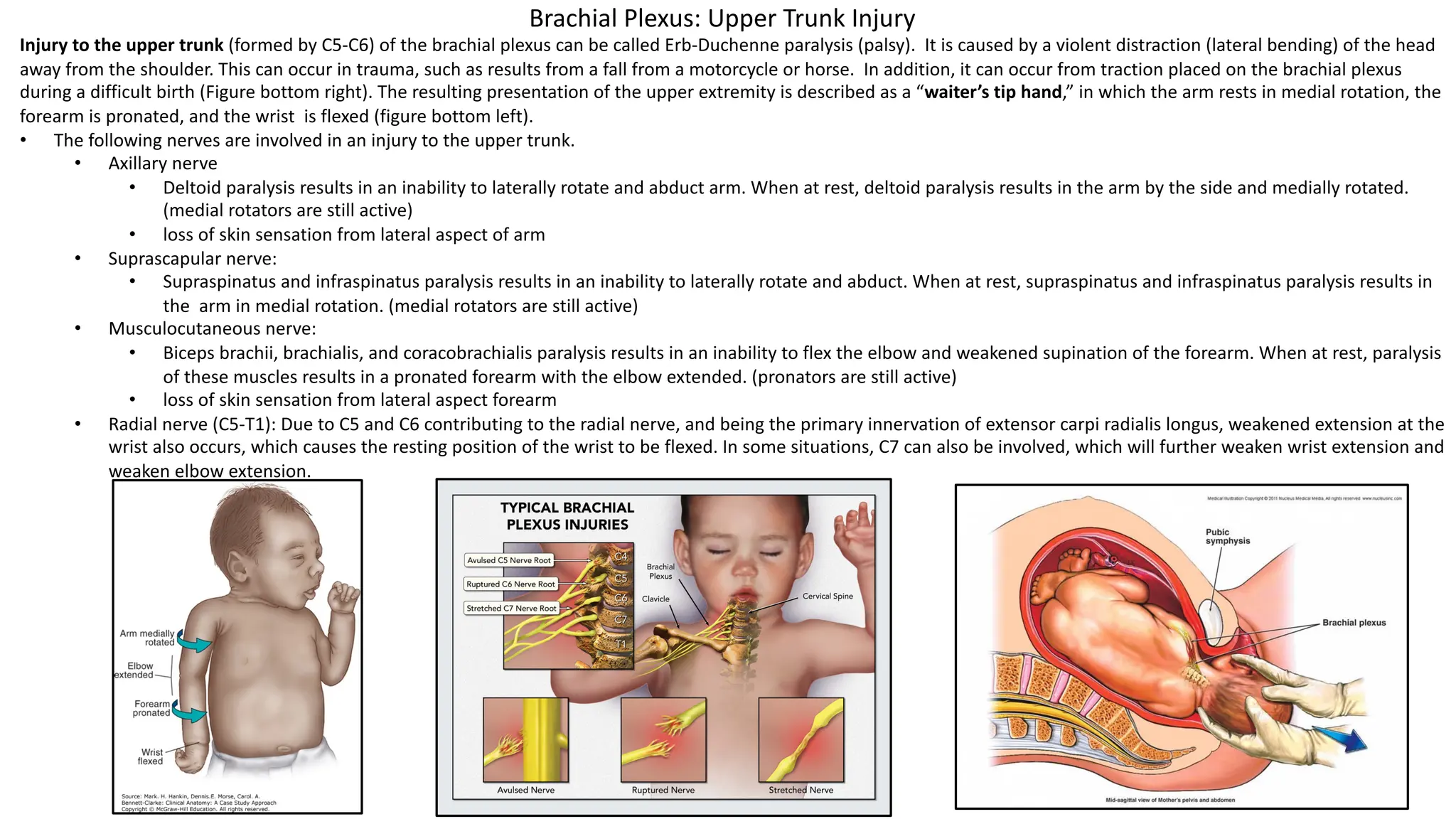
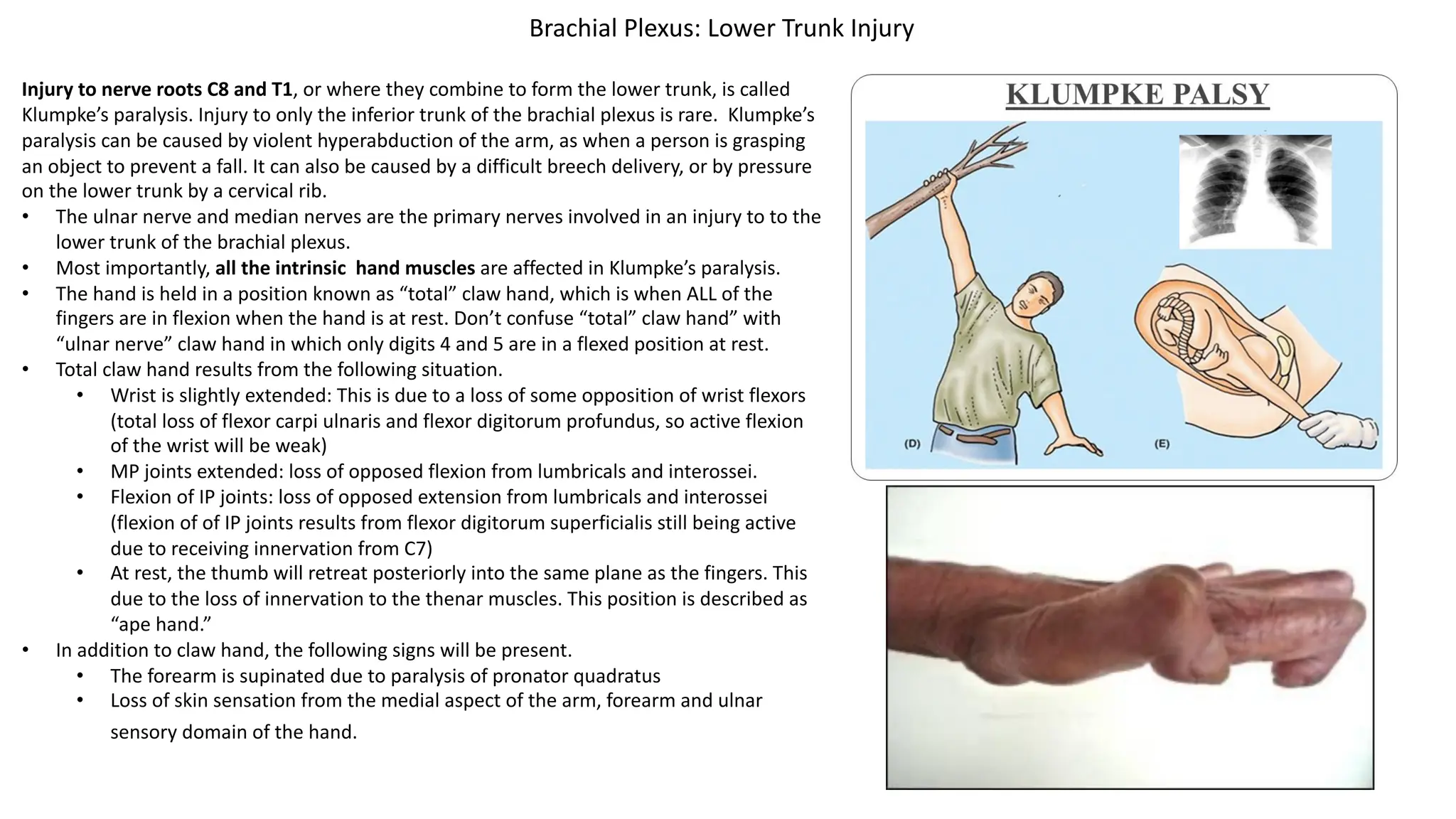
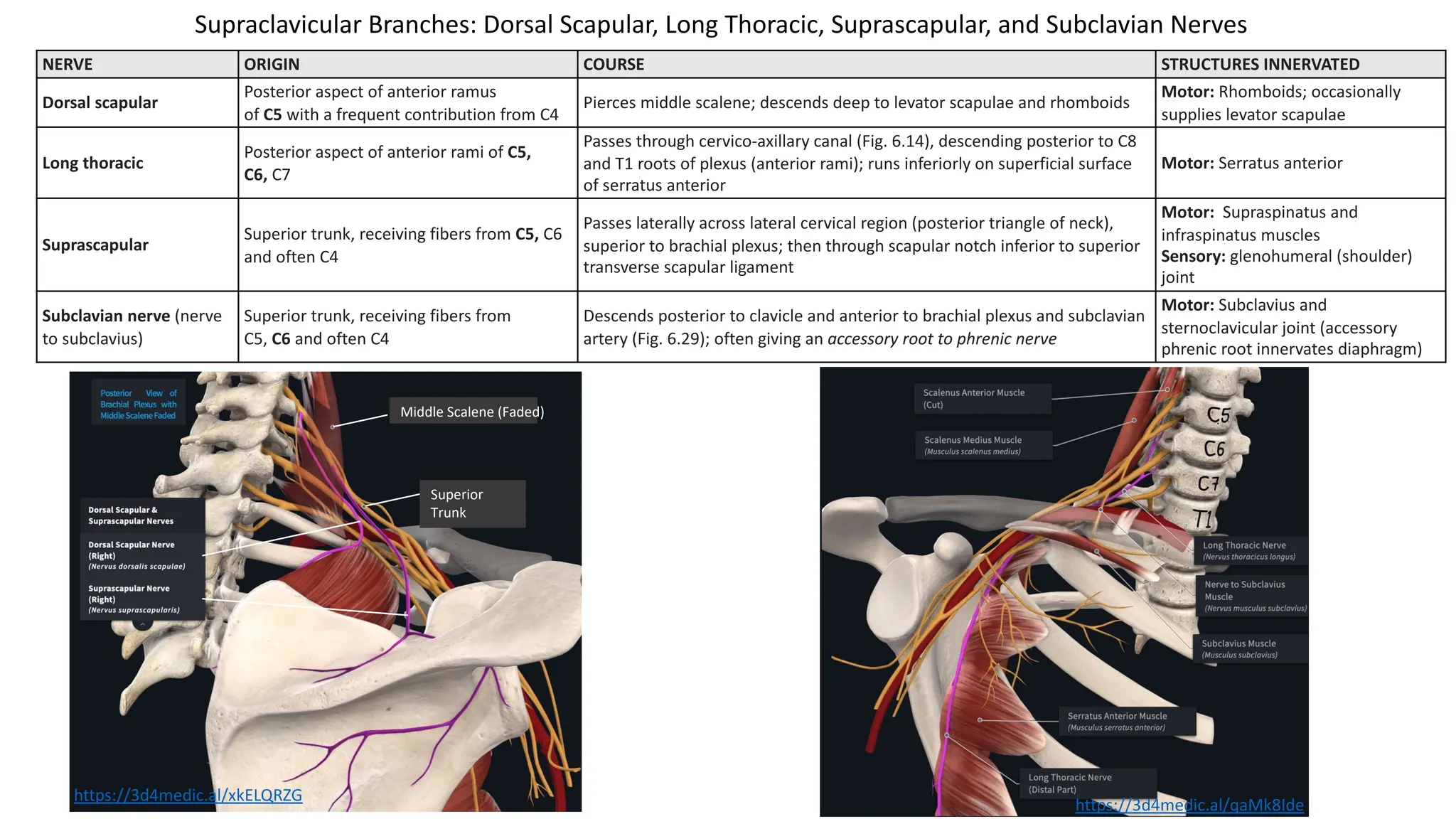
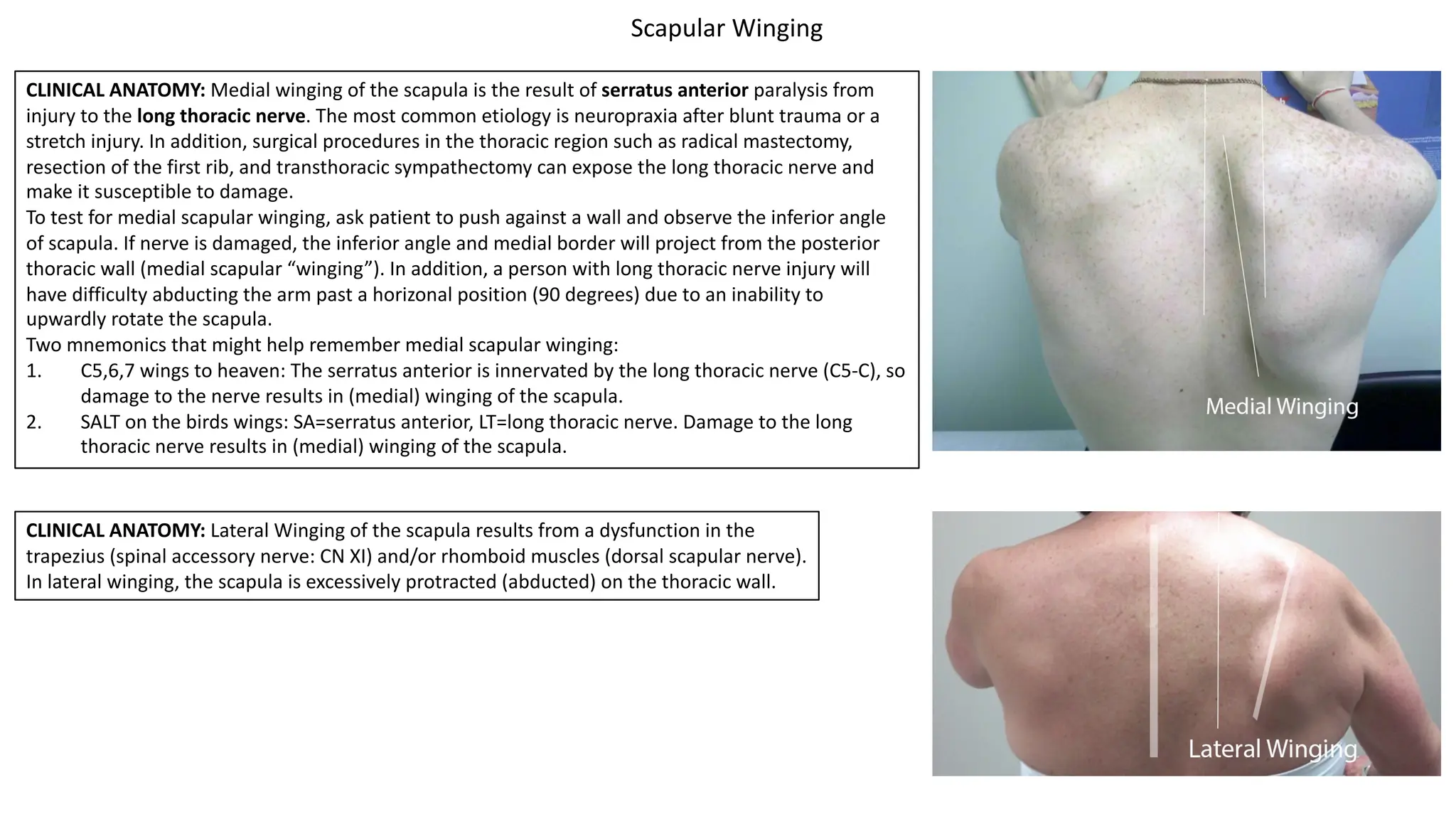
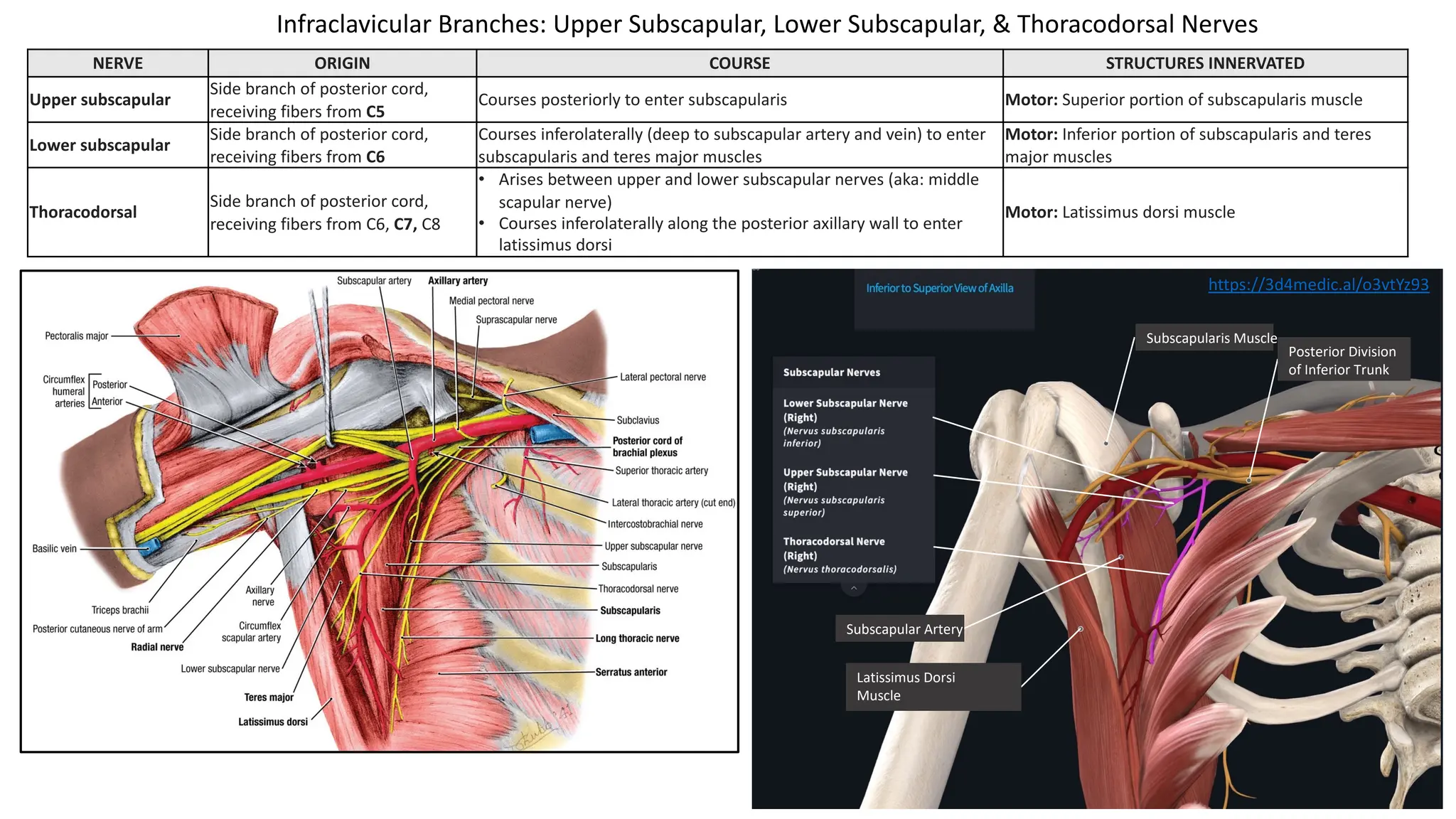
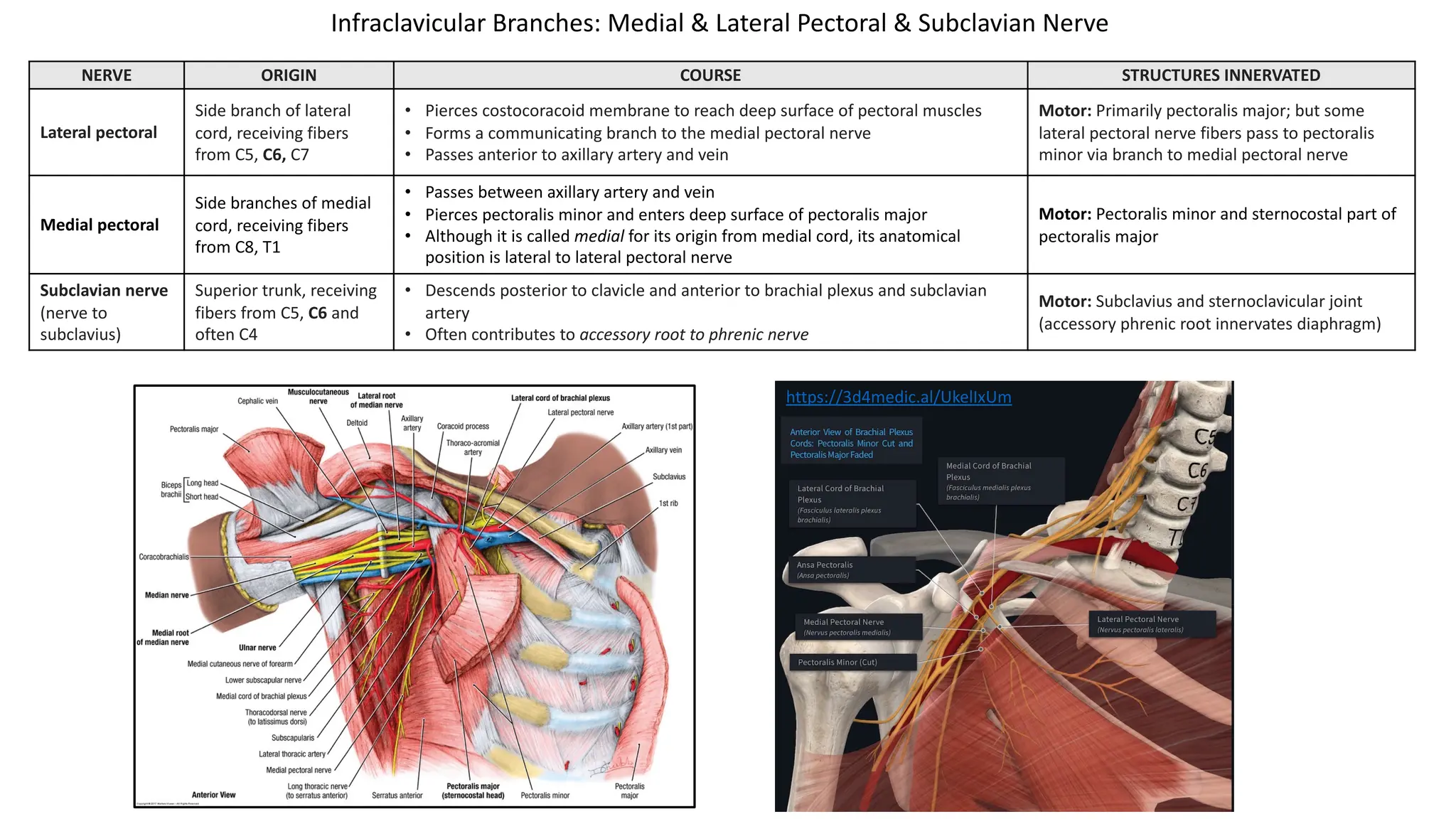
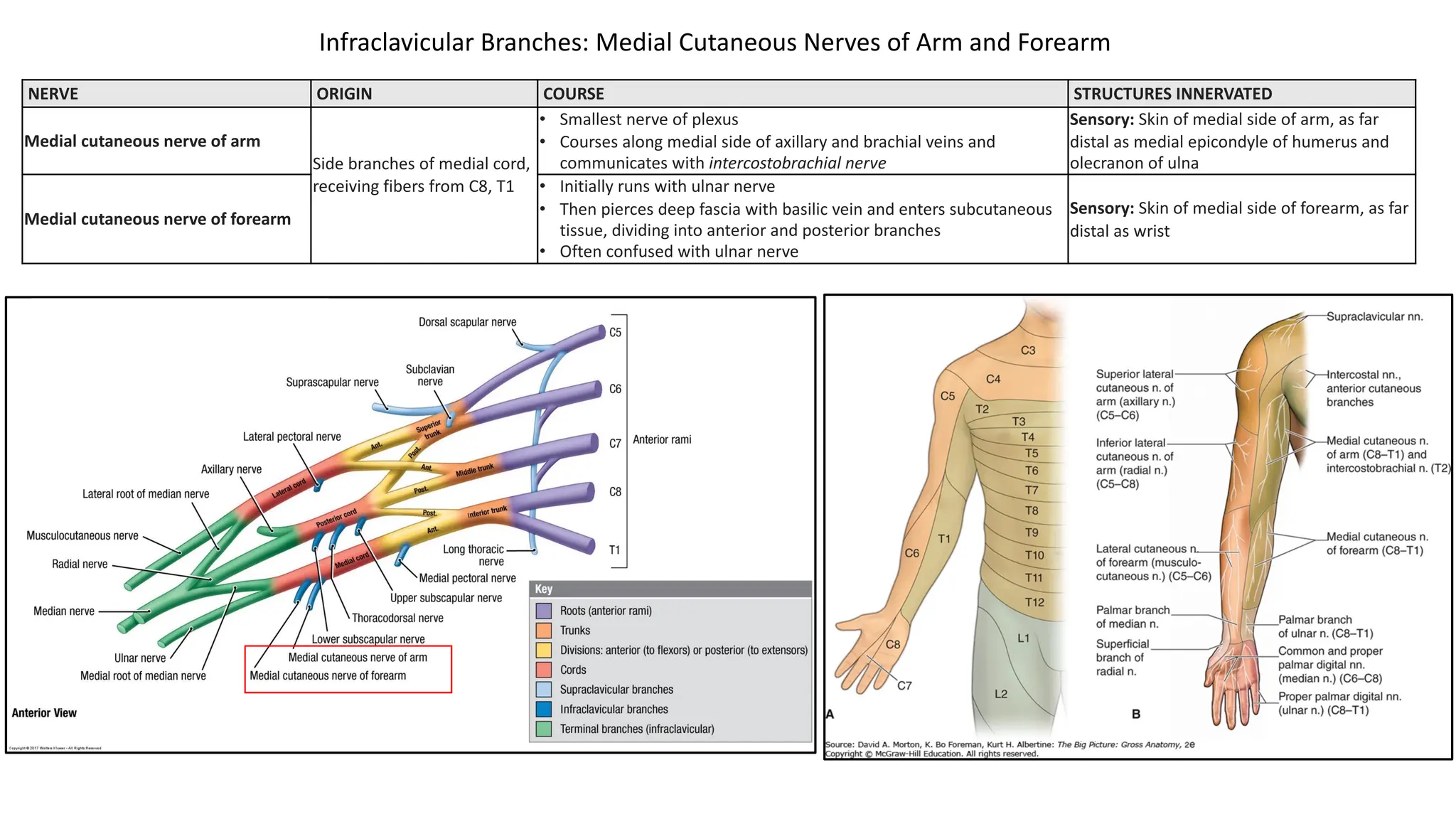
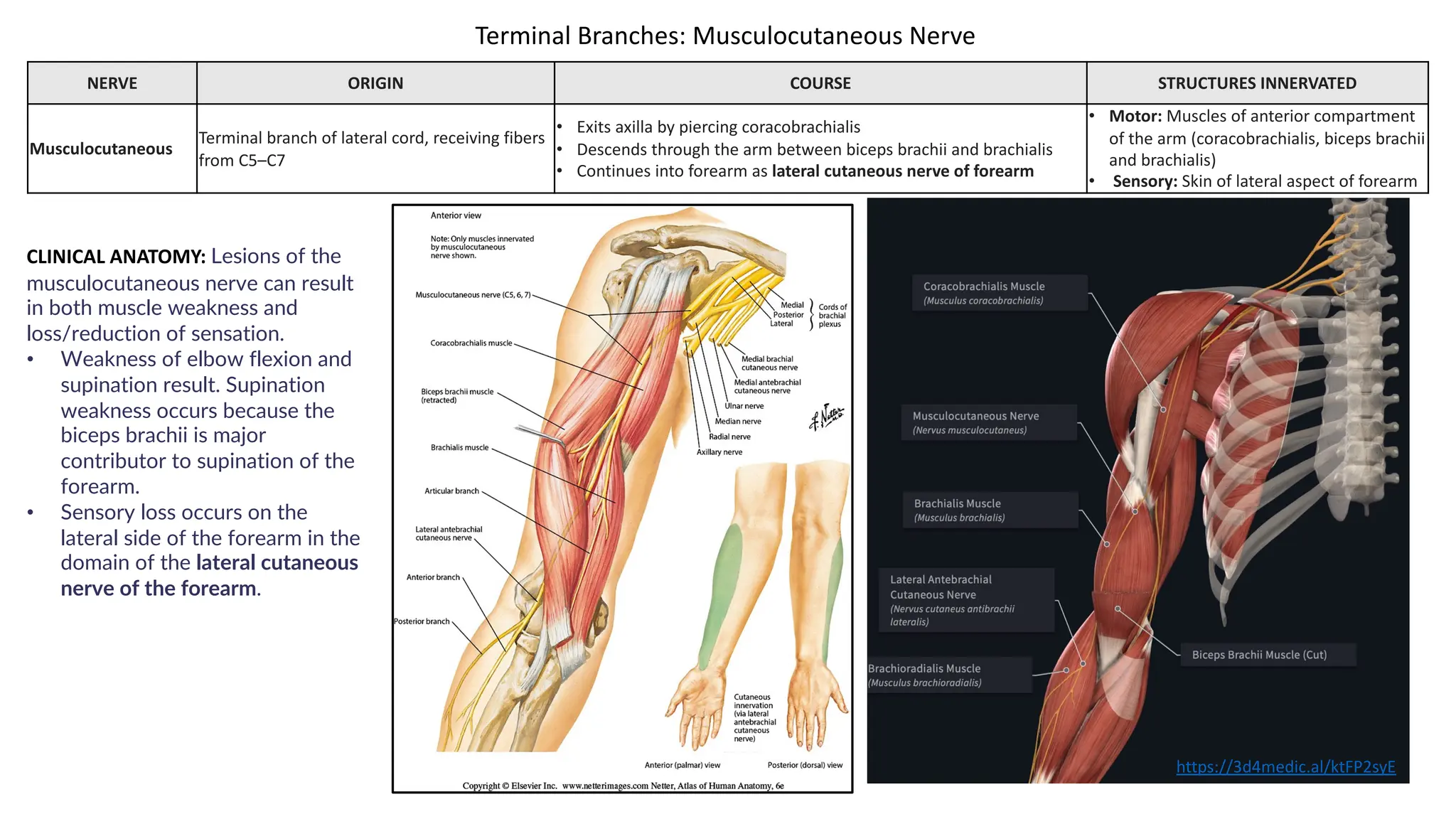
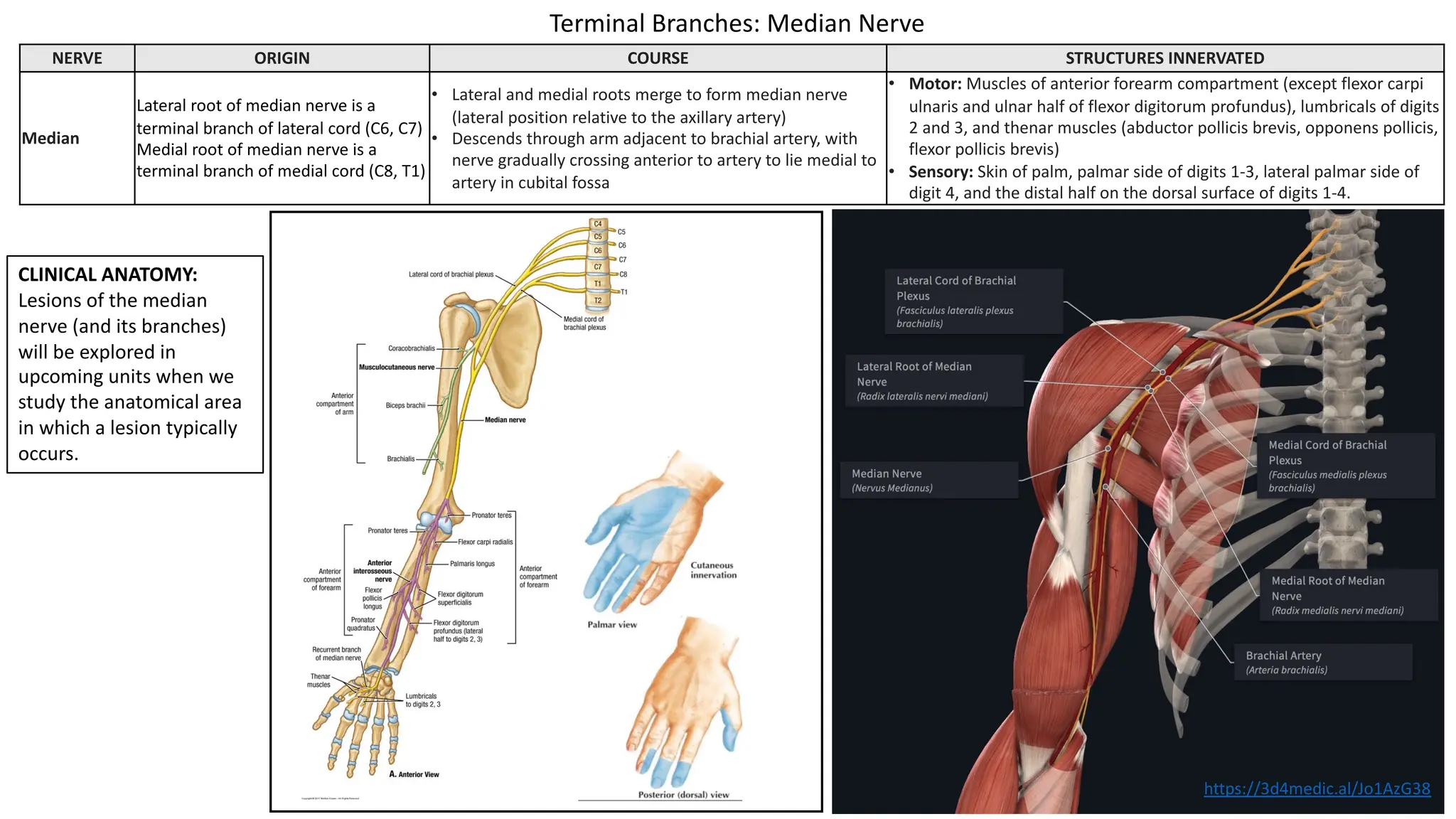
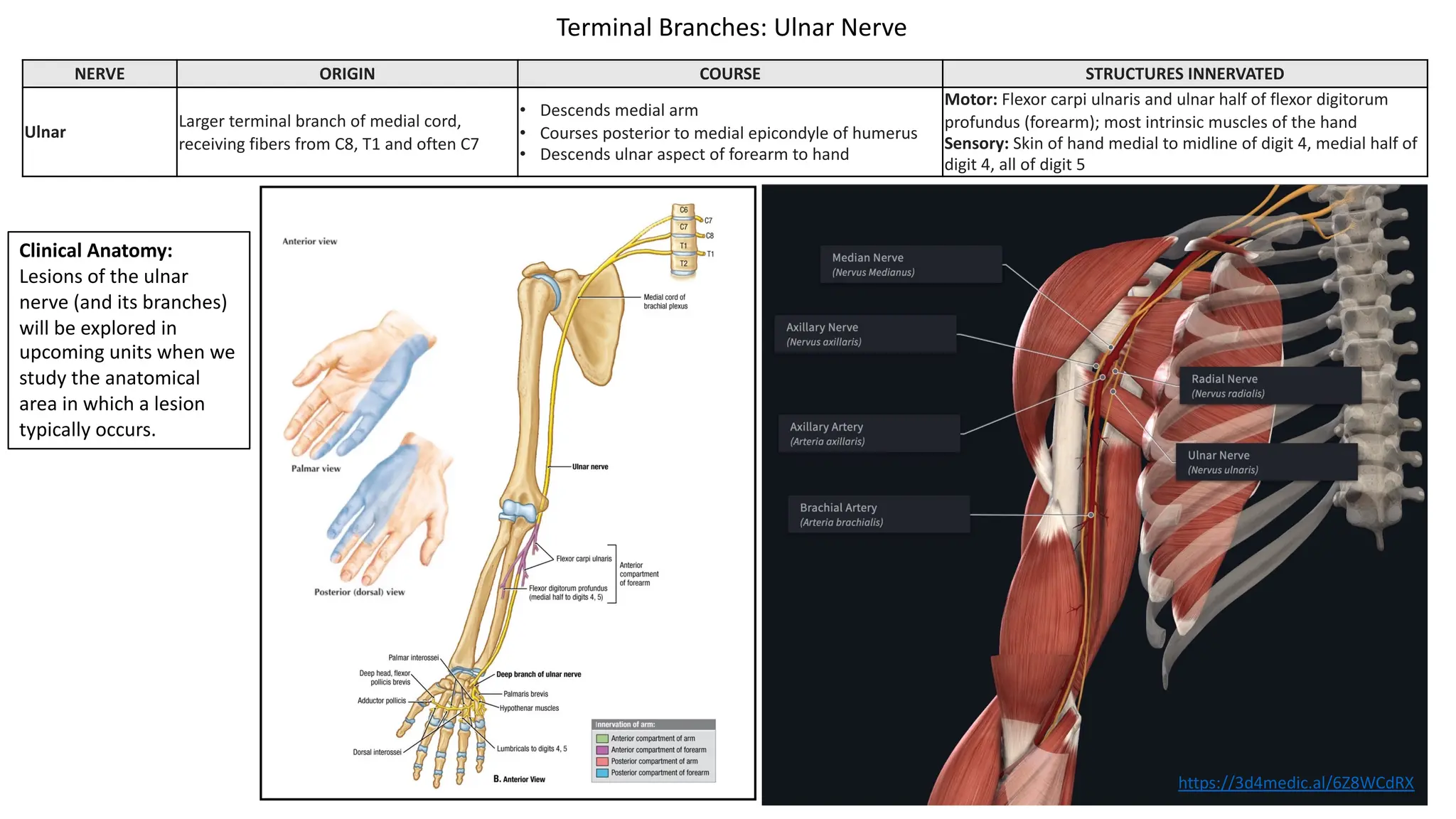
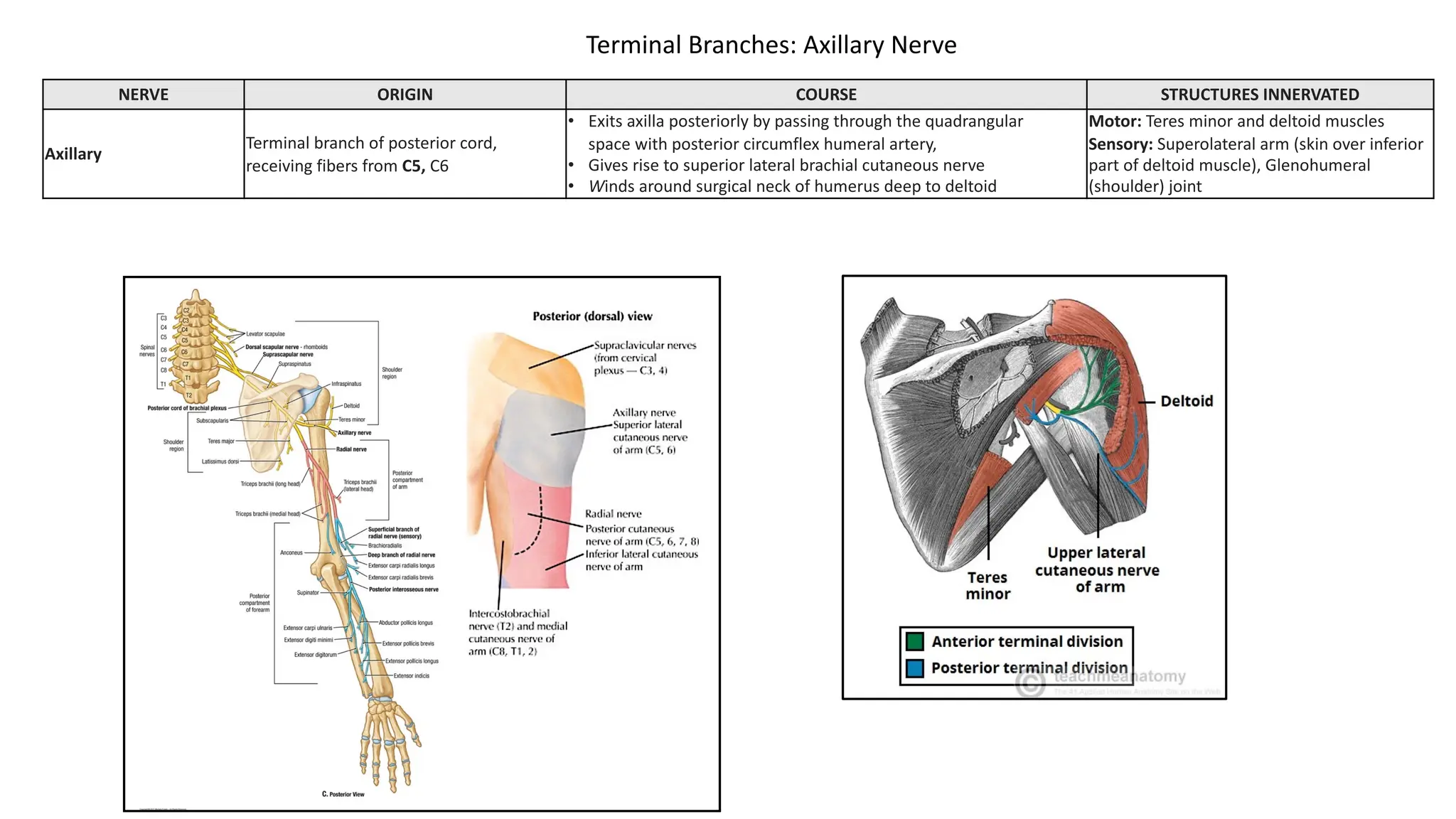
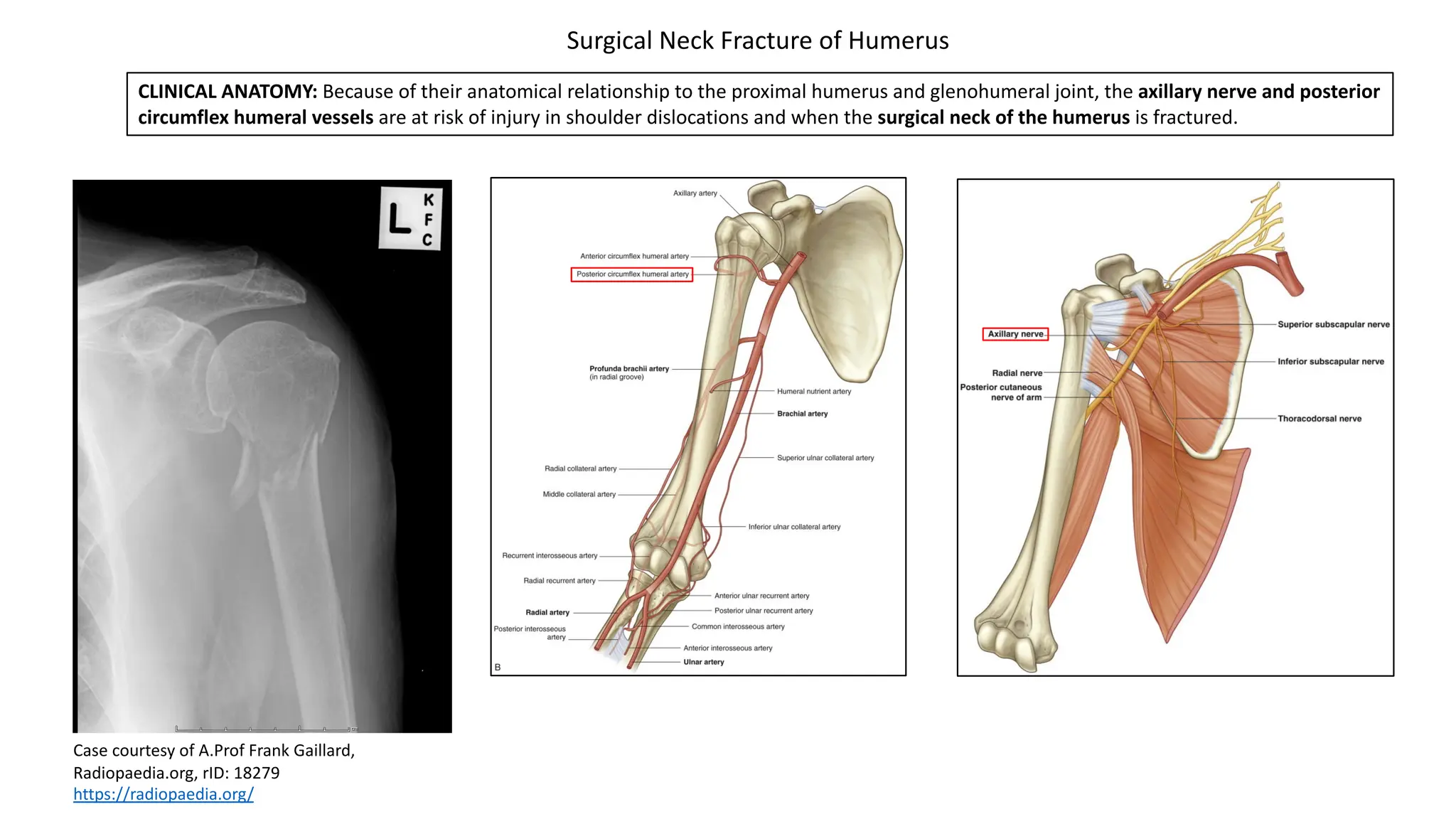
The document provides an overview of the axilla and brachial plexus anatomy, detailing structures such as the axillary artery, axillary vein, lymph nodes, and branches of the brachial plexus. It discusses injuries related to the upper and lower trunks of the brachial plexus, including their causes, associated symptoms, and the specific nerves affected. Additionally, it covers lymphatic drainage routes from the upper limb and explains clinical conditions like scapular winging due to nerve injuries.