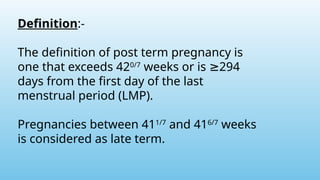
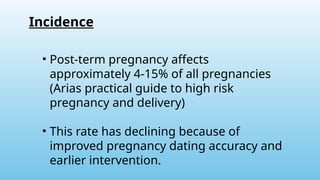
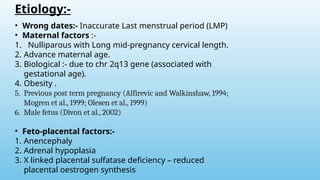
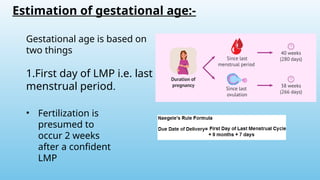
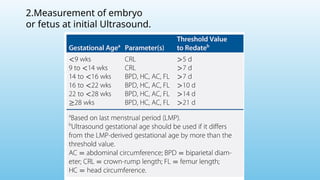
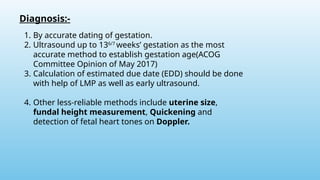
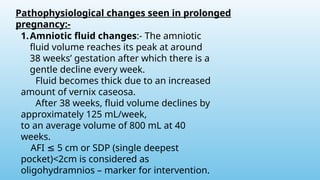
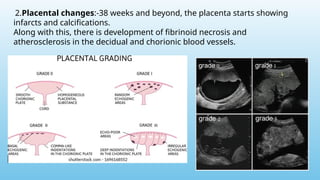
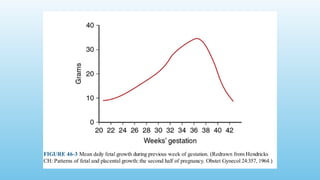
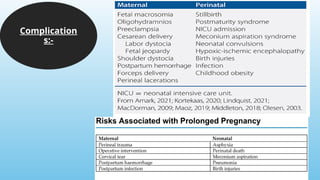
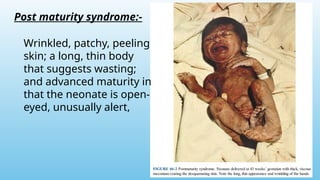
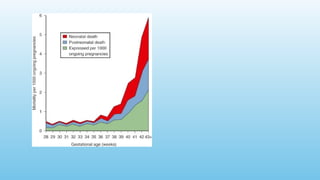
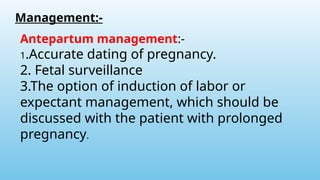
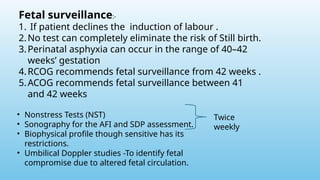
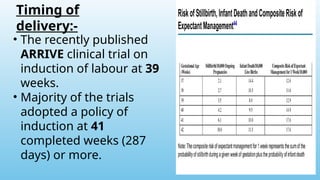
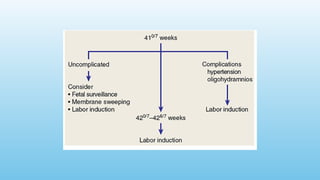
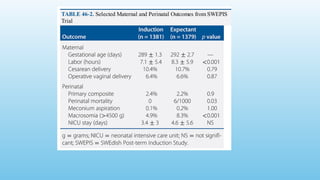
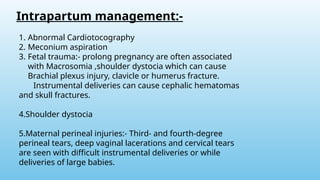
This presentation provides an in-depth overview of Post-Term Pregnancy, a condition where pregnancy extends beyond 42 completed weeks of gestation. It discusses the definition, epidemiology, etiological factors, maternal and fetal risks, clinical features, methods of diagnosis, and management strategies. The slide deck also highlights complications such as macrosomia, oligohydramnios, and increased perinatal morbidity, along with current guidelines on induction of labor and monitoring. Designed for medical students, obstetricians, gynecologists, and healthcare professionals, this resource emphasizes the importance of timely diagnosis and evidence-based management to ensure safe outcomes for both mother and baby.