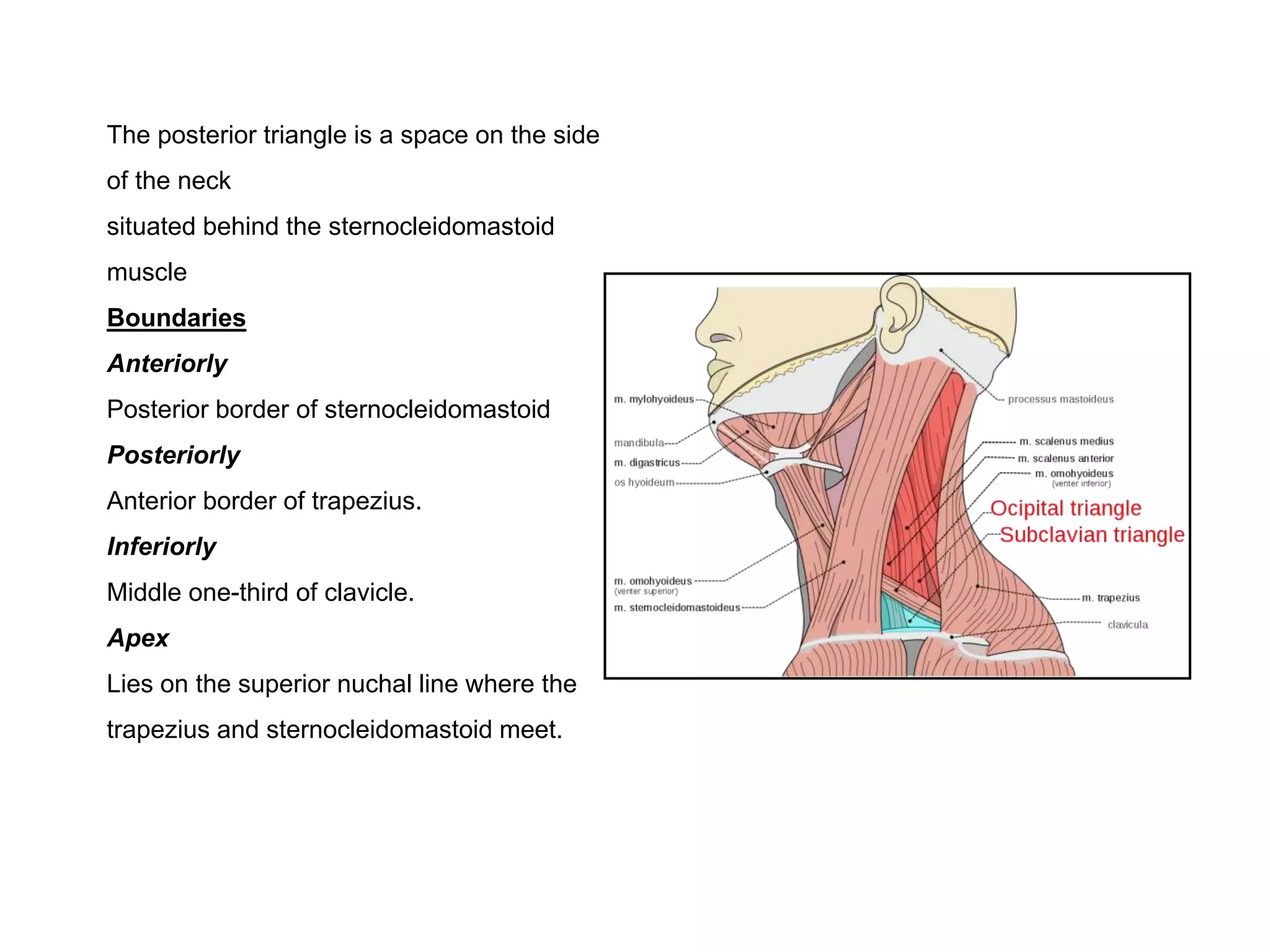
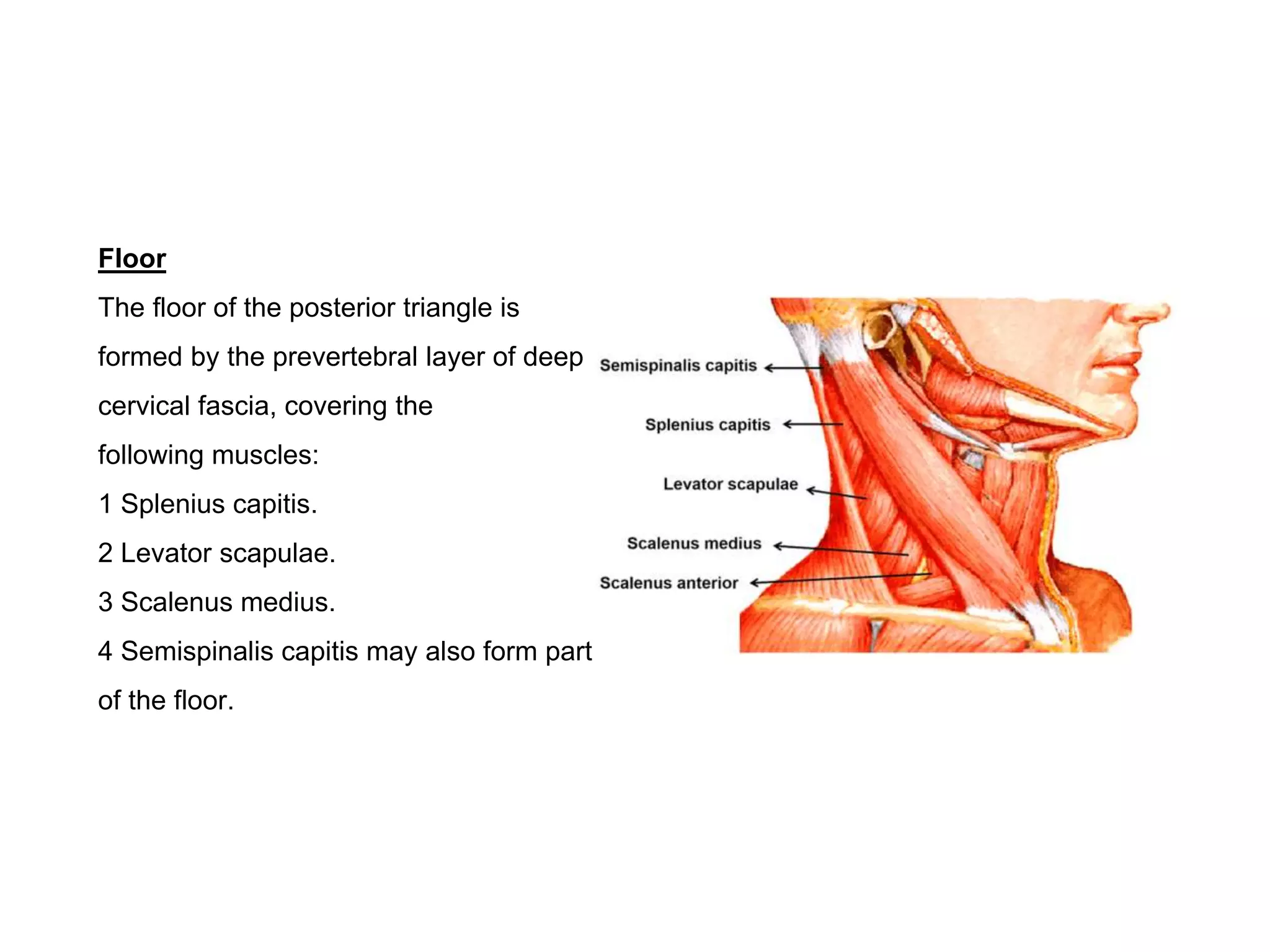
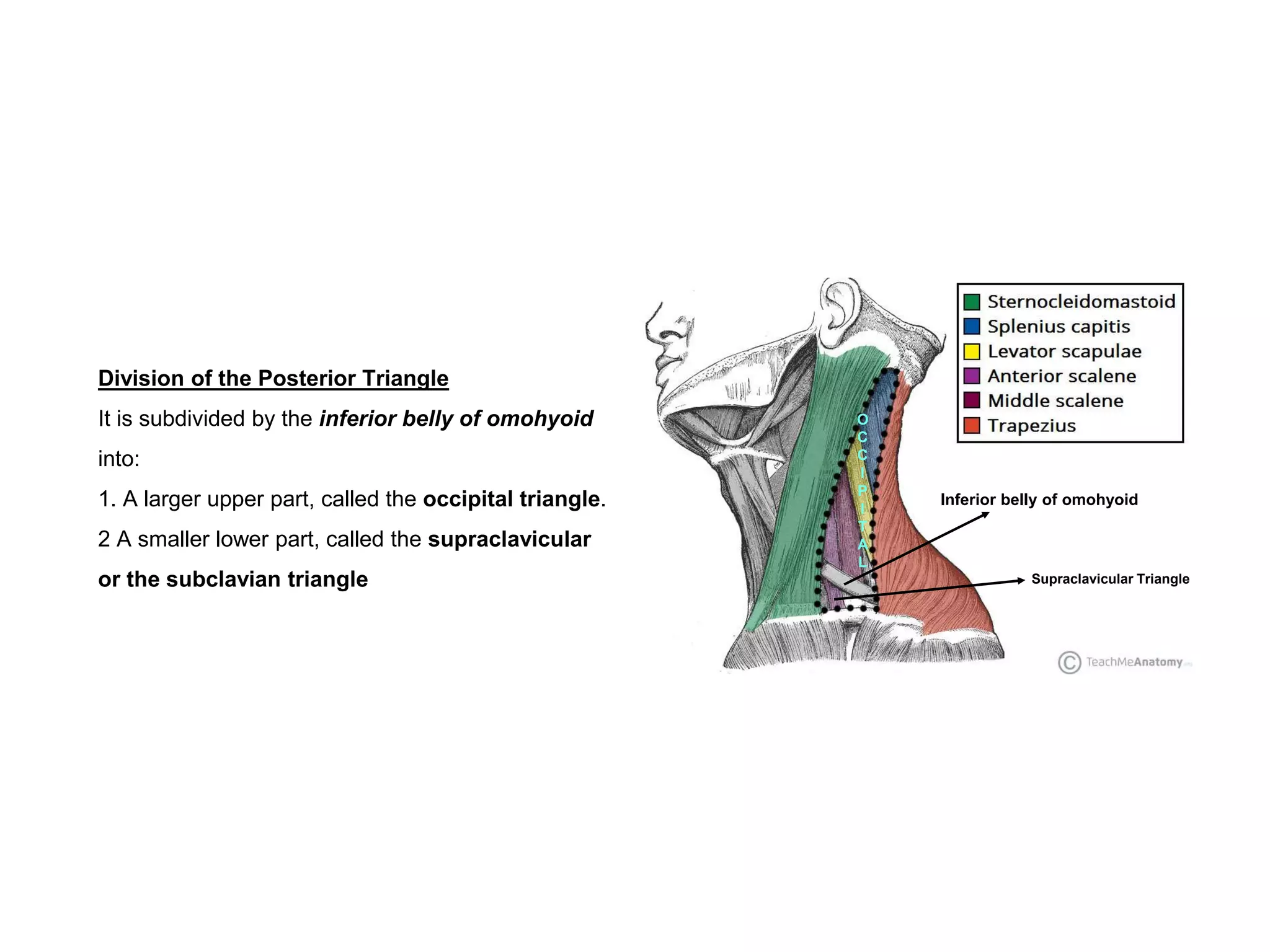
The posterior triangle is a space on the side of the neck bounded anteriorly by the sternocleidomastoid muscle, posteriorly by the trapezius muscle, and inferiorly by the middle third of the clavicle. It is divided into the occipital triangle and supraclavicular triangle by the omohyoid muscle. The occipital triangle contains nerves like the spinal accessory nerve and branches of the cervical plexus. The supraclavicular triangle contains structures of the brachial plexus like the trunks and nerves to muscles like serratus anterior. Lymph nodes in the posterior triangle drain the neck.