This document summarizes the AIDS epidemic in Eastern and Southern Africa and progress towards meeting international targets on HIV/AIDS. Some key points:
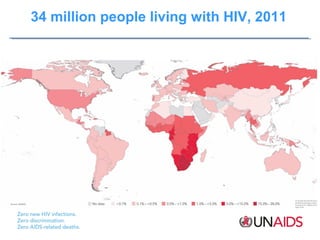
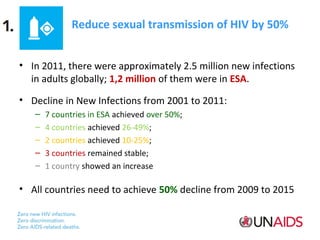
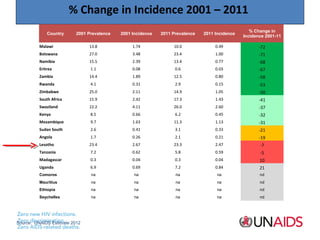
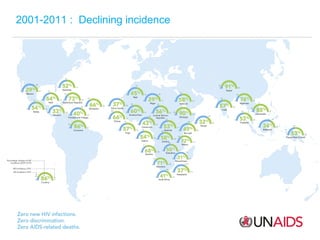
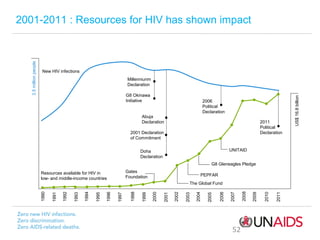
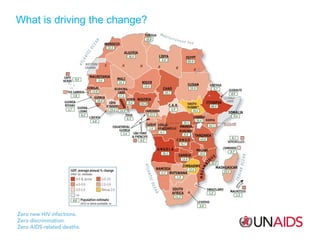
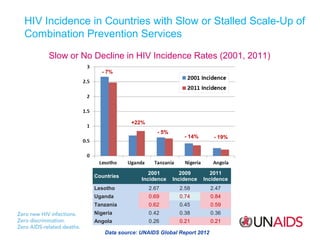
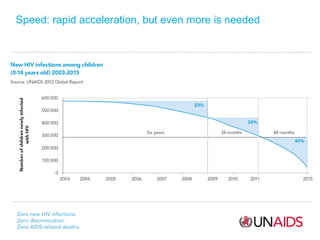
1) There are 34 million people living with HIV globally in 2011, with 1.2 million new infections in Eastern and Southern Africa. Several countries have reduced new infections by over 50% since 2001.
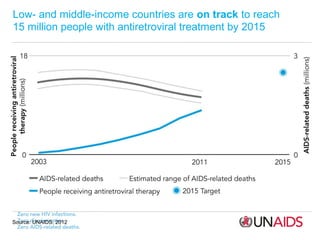
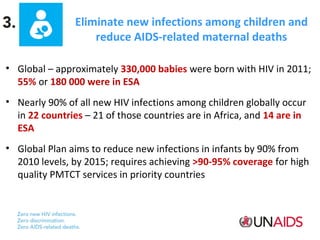
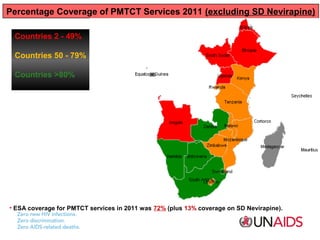
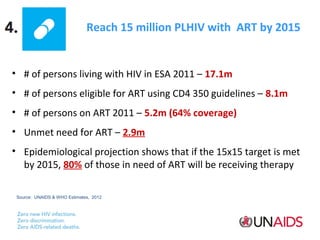
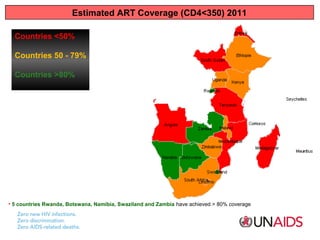
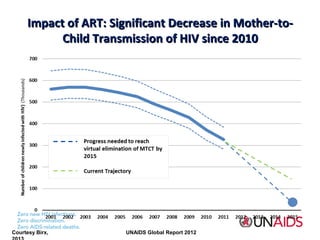
2) Coverage of prevention of mother-to-child transmission services was 72% in 2011 in the region. 5.2 million people were receiving antiretroviral treatment out of 8.1 million estimated to be eligible.
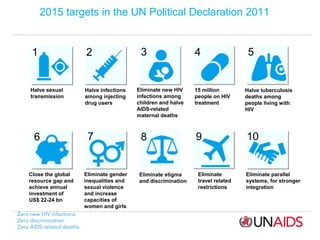
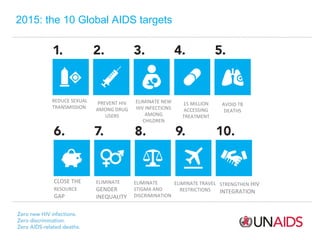
3) Reducing sexual transmission by 50% and reaching 15 million people on HIV treatment by 2015 are among key global targets, but

![Community support keeps people on treatment
CLINIC-BASED TREATMENT
70%
still receiving treatment after two years
Sub-Saharan Africa: people
receiving ART from specialist
clinics
Source: Fox MP, Rosen S. Patient retention in antiretroviral therapy programs up to three years on treatment in subSaharan Africa, 2007–2009: systematic review. Tropical Medicine and International Health, 2010, 15(Suppl. 1):1–15.
COMMUNITY TREATMENT MODEL
98%
still receiving treatment after two years
Mozambique: self-initiated
community model
Source: Decroo T et al. Distribution of antiretroviral treatment through self-forming groups of patients in Tete province,
Mozambique. Journal of Acquired Immune Deficiency Syndromes, 2010 [Epub ahead of print].](https://image.slidesharecdn.com/post2015agendaaidscoordination-131108132753-phpapp01/85/Post-2015-agenda-aids-coordination-29-320.jpg)


![Community support keeps people on treatment
CLINIC-BASED TREATMENT
70%
still receiving treatment after two years
Sub-Saharan Africa: people
receiving ART from specialist
clinics
Source: Fox MP, Rosen S. Patient retention in antiretroviral therapy programs up to three years on treatment in subSaharan Africa, 2007–2009: systematic review. Tropical Medicine and International Health, 2010, 15(Suppl. 1):1–15.
COMMUNITY TREATMENT MODEL
98%
still receiving treatment after two years
Mozambique: self-initiated
community model
Source: Decroo T et al. Distribution of antiretroviral treatment through self-forming groups of patients in Tete province,
Mozambique. Journal of Acquired Immune Deficiency Syndromes, 2010 [Epub ahead of print].
Sources: Fox MP, Rosen S. Tropical Medicine and International Health, 2010;
Decroo T et al. Journal of Acquired Immune Deficiency Syndromes, 2010.](https://image.slidesharecdn.com/post2015agendaaidscoordination-131108132753-phpapp01/85/Post-2015-agenda-aids-coordination-61-320.jpg)