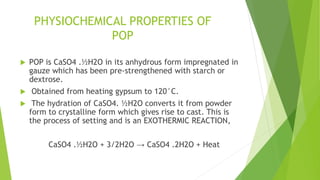
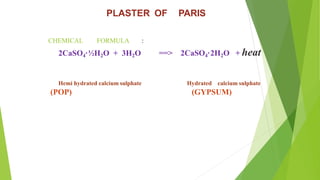
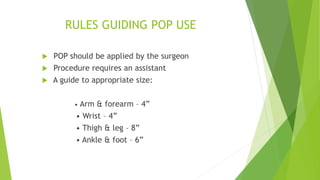
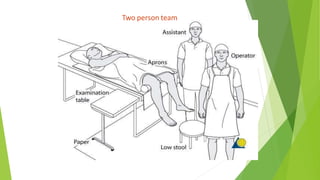
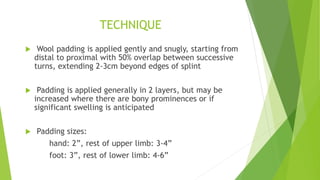
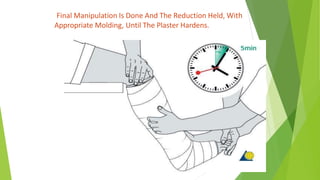
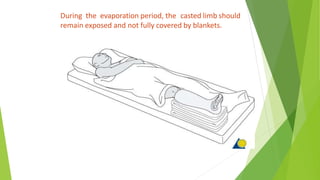
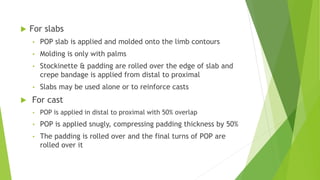
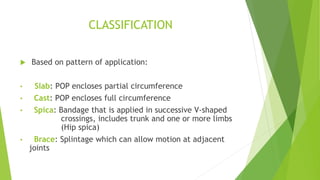
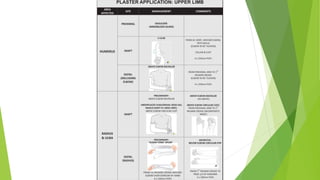
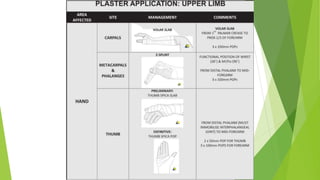
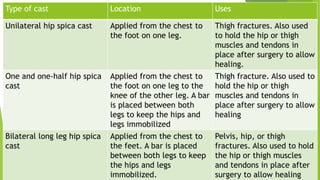
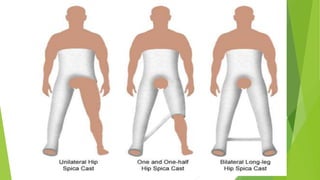
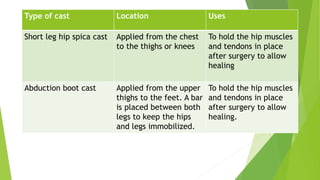
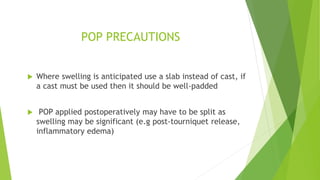
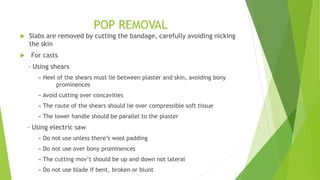
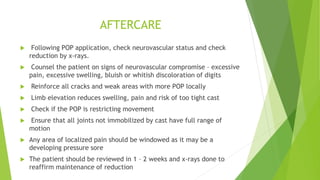
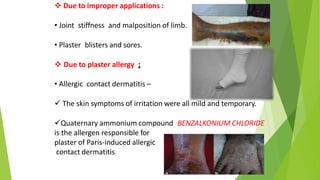
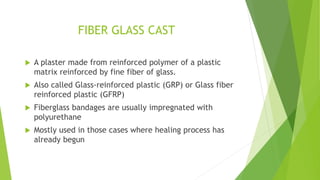
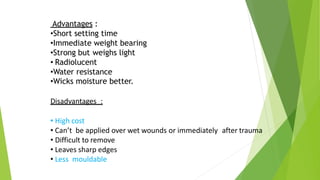
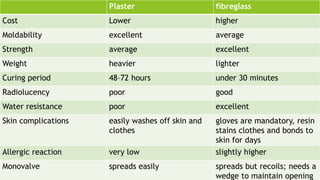
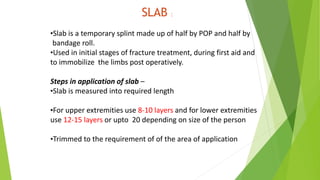
This document discusses the properties, application techniques, and complications of Plaster of Paris (POP) in orthopedic practice, emphasizing its importance in immobilizing fractures and musculoskeletal injuries. It outlines the chemical process of POP, casting techniques, guidelines for application and removal, precautions, alternatives, and potential complications. The text serves as a comprehensive guide for surgeons and healthcare practitioners involved in the application of POP for fracture and injury management.