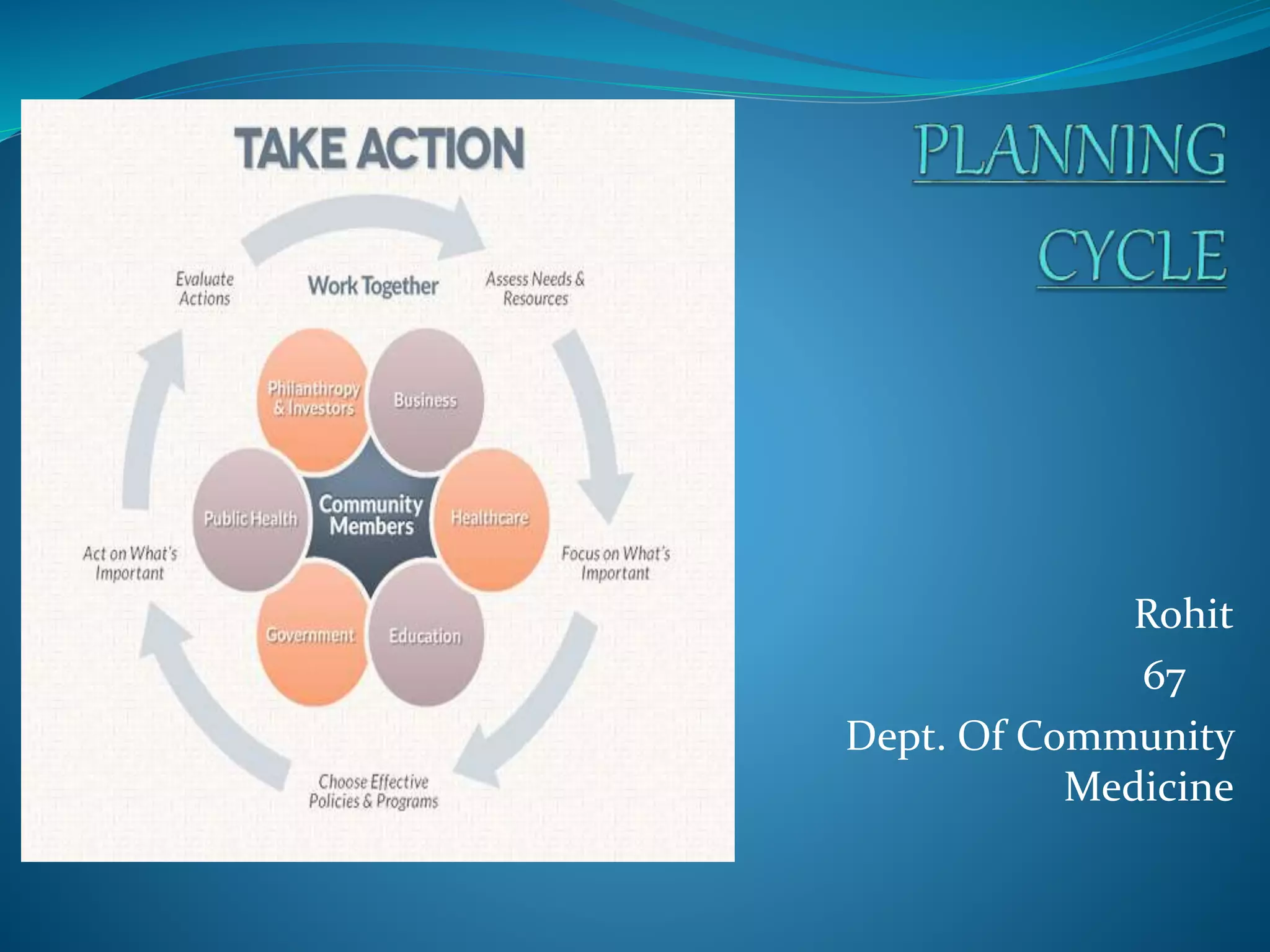
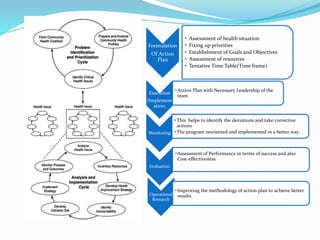
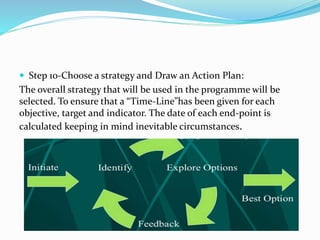
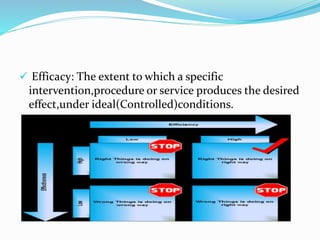
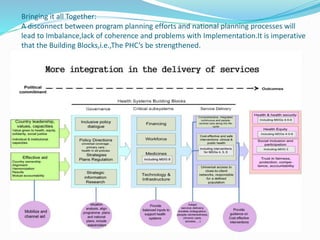
The document outlines a systematic health planning process that includes identifying health problems, assessing resources, and engaging community participation. It highlights various steps such as situational analysis, prioritization of needs, setting objectives, and evaluating program effectiveness, specifically in the context of malaria control in India. The strategic plan aims to reduce malaria cases and mortality through targeted interventions and community involvement by 2017.