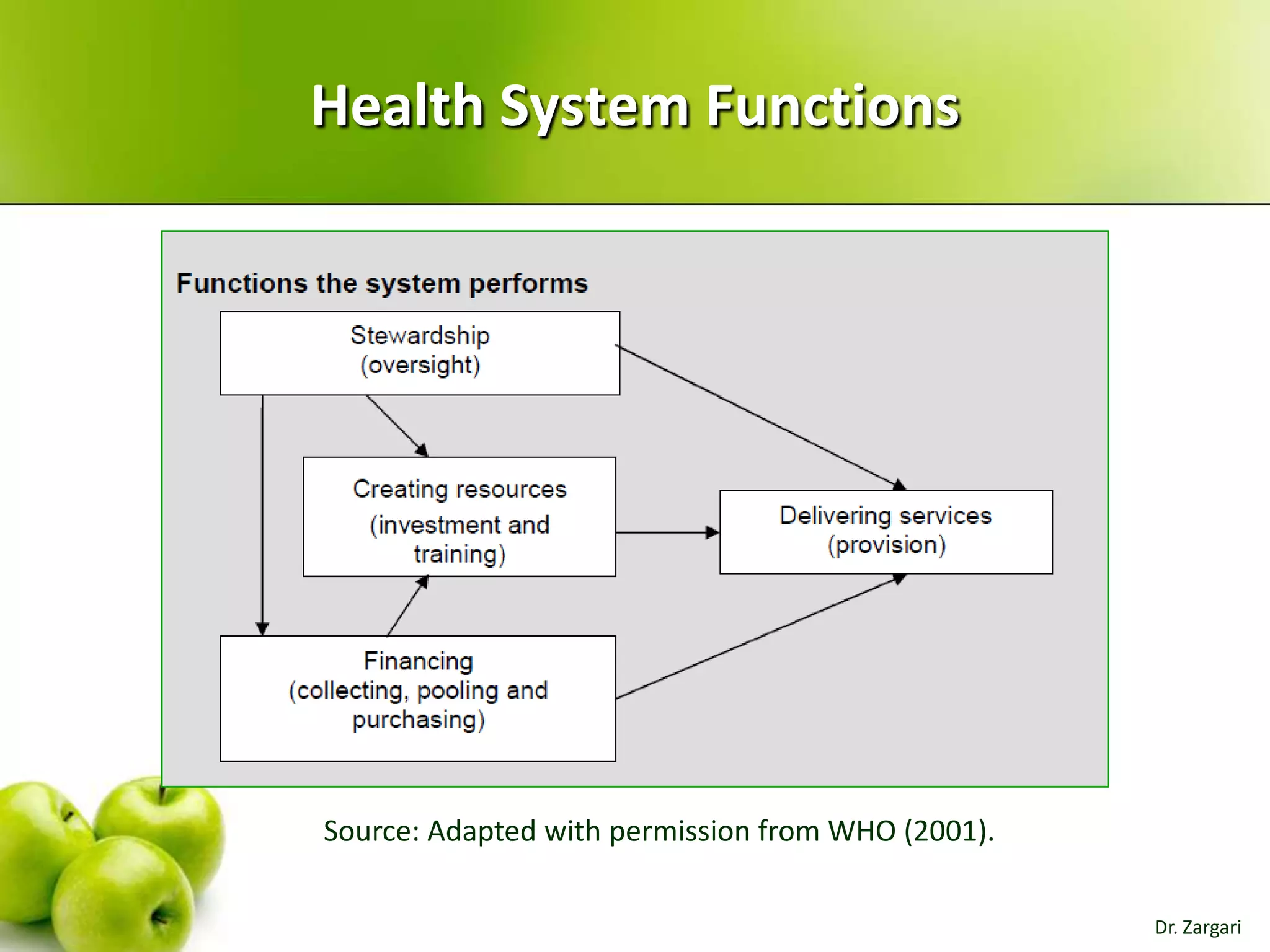
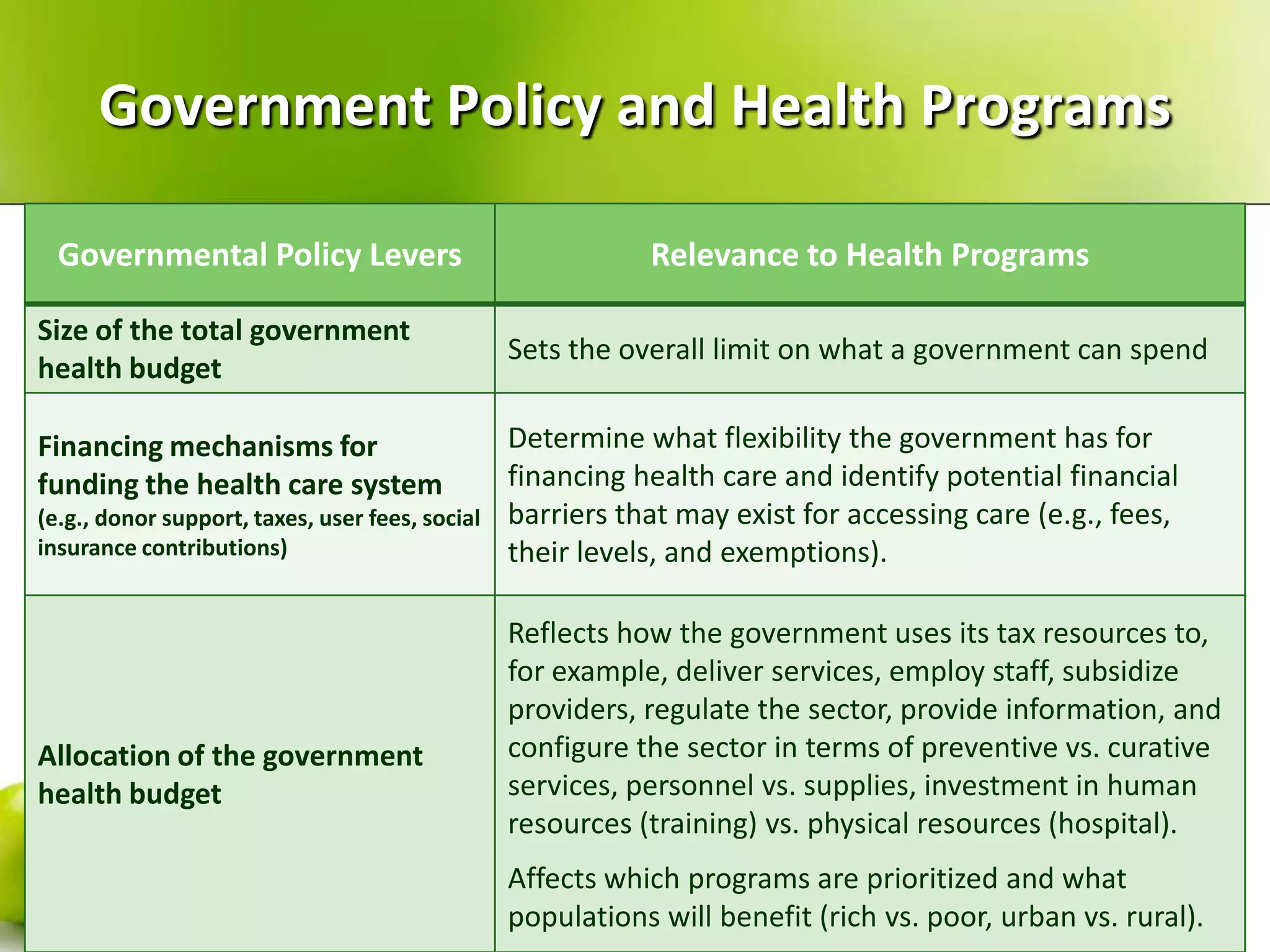
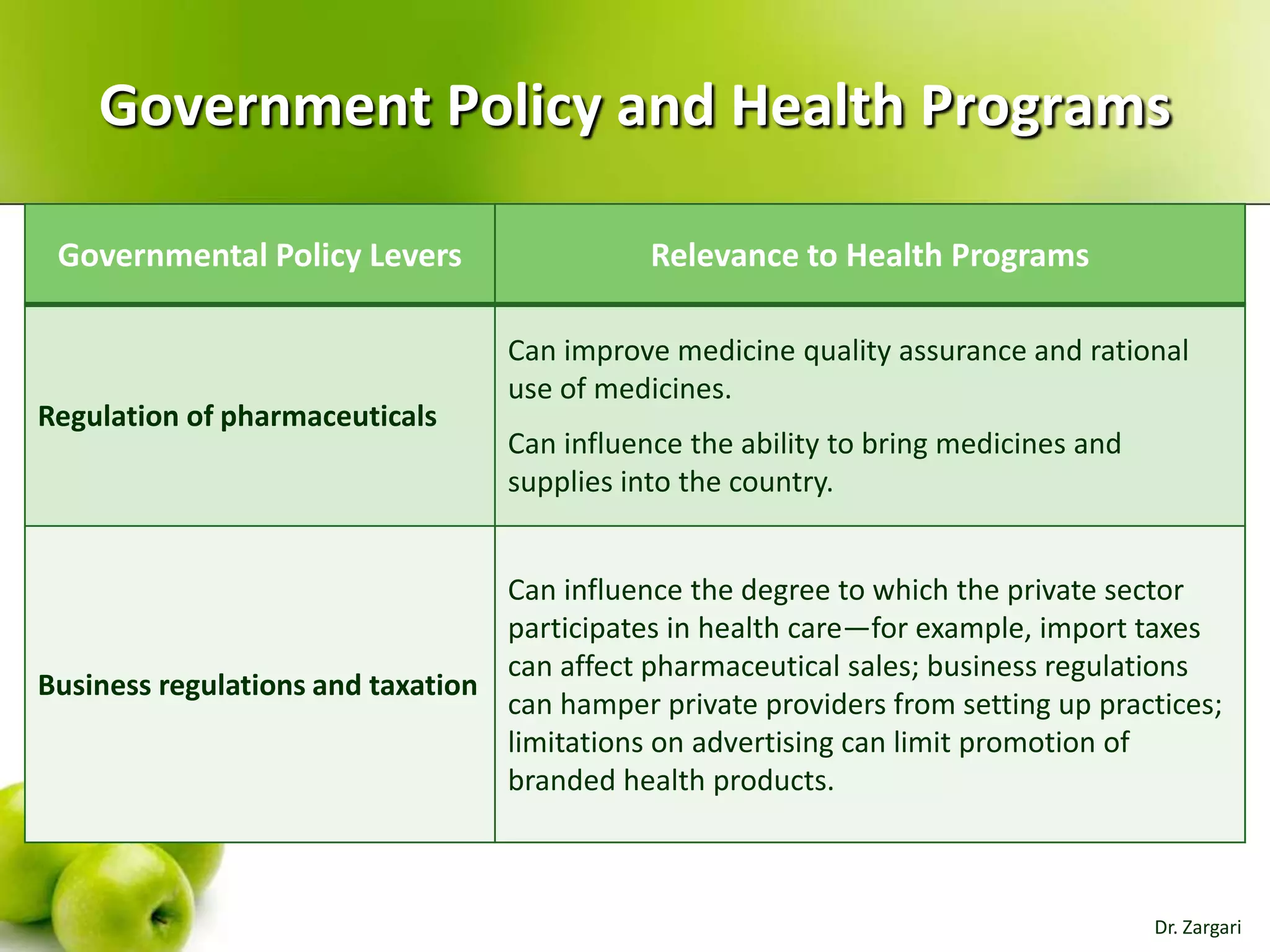
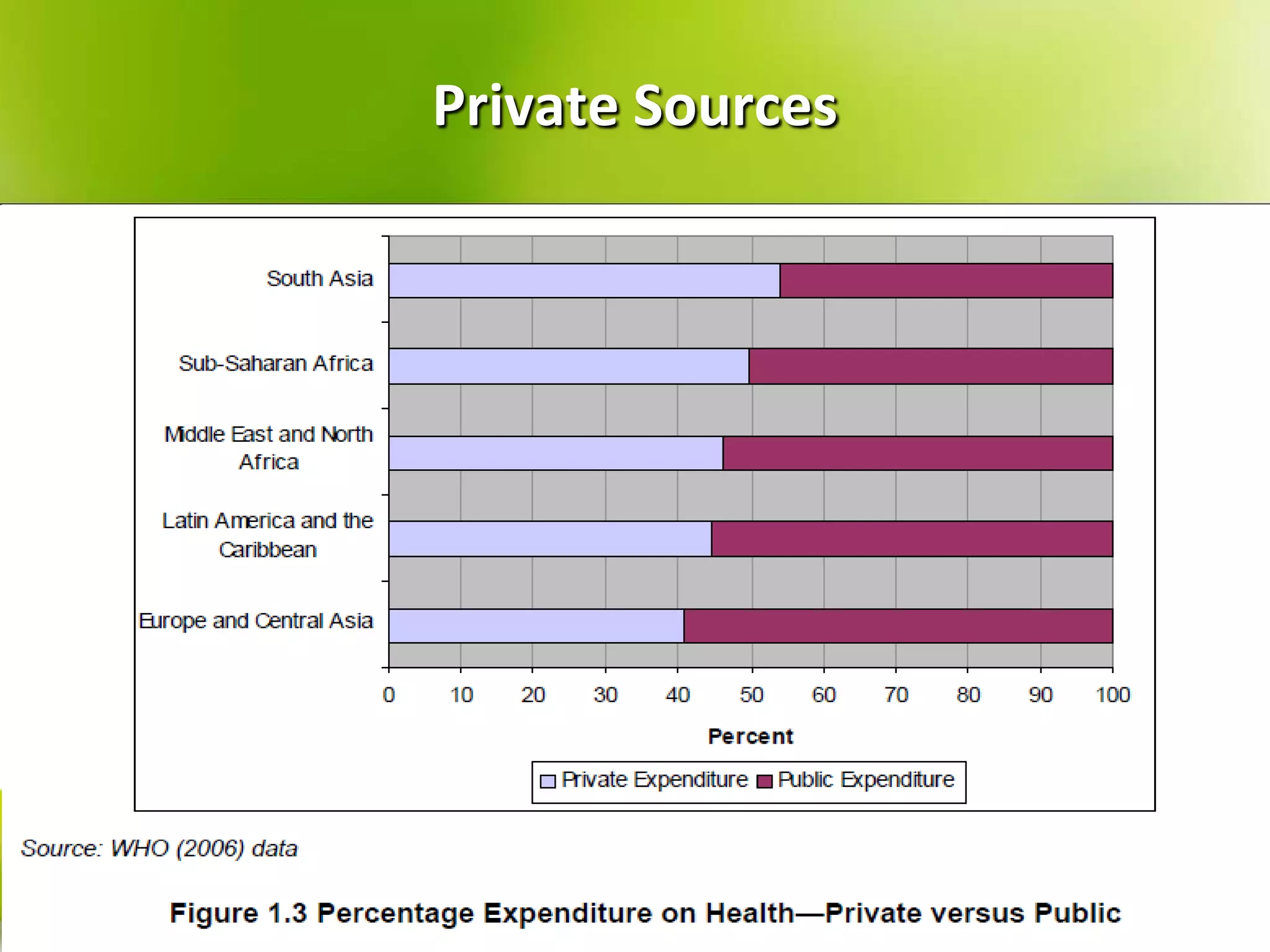
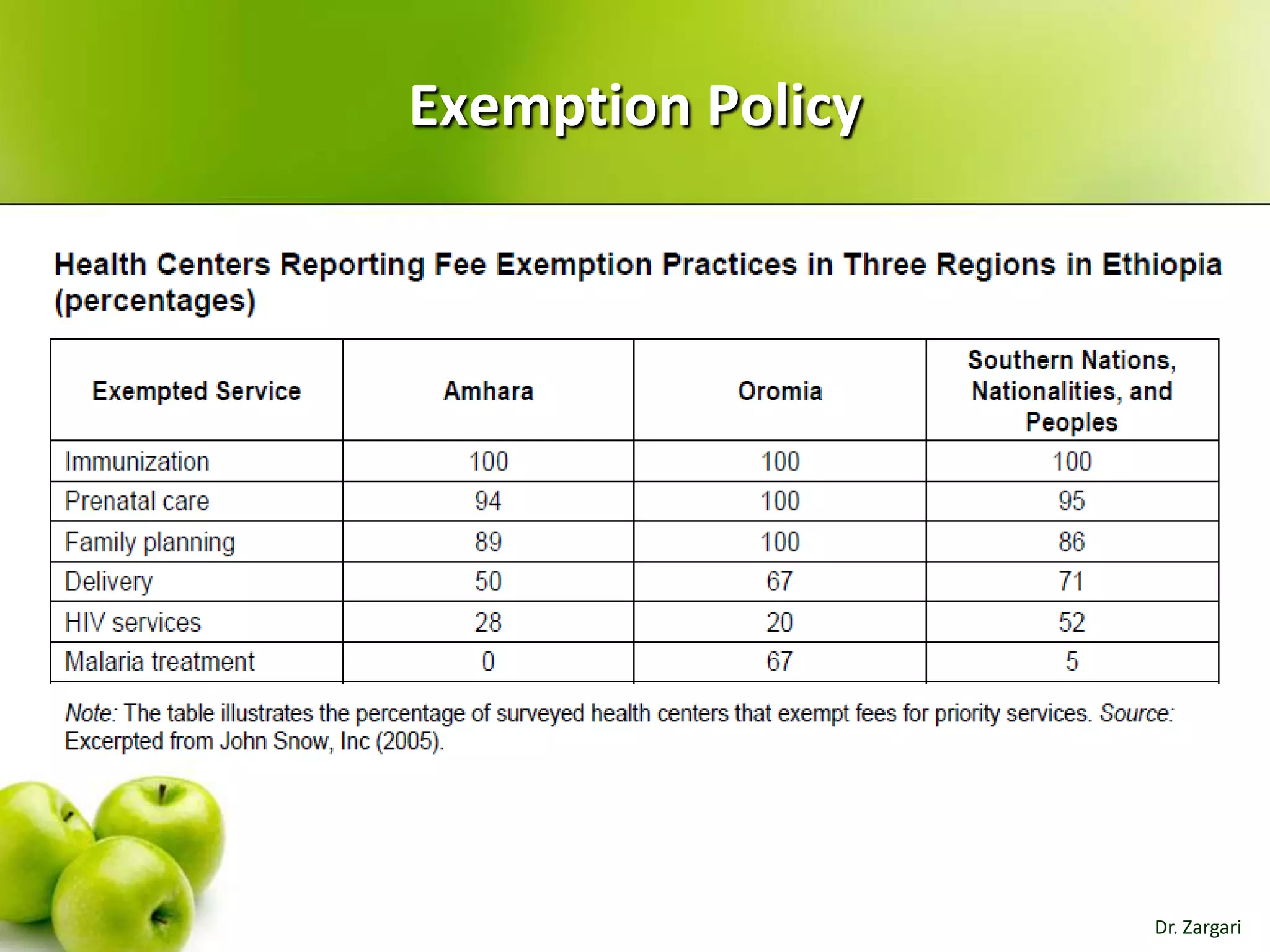
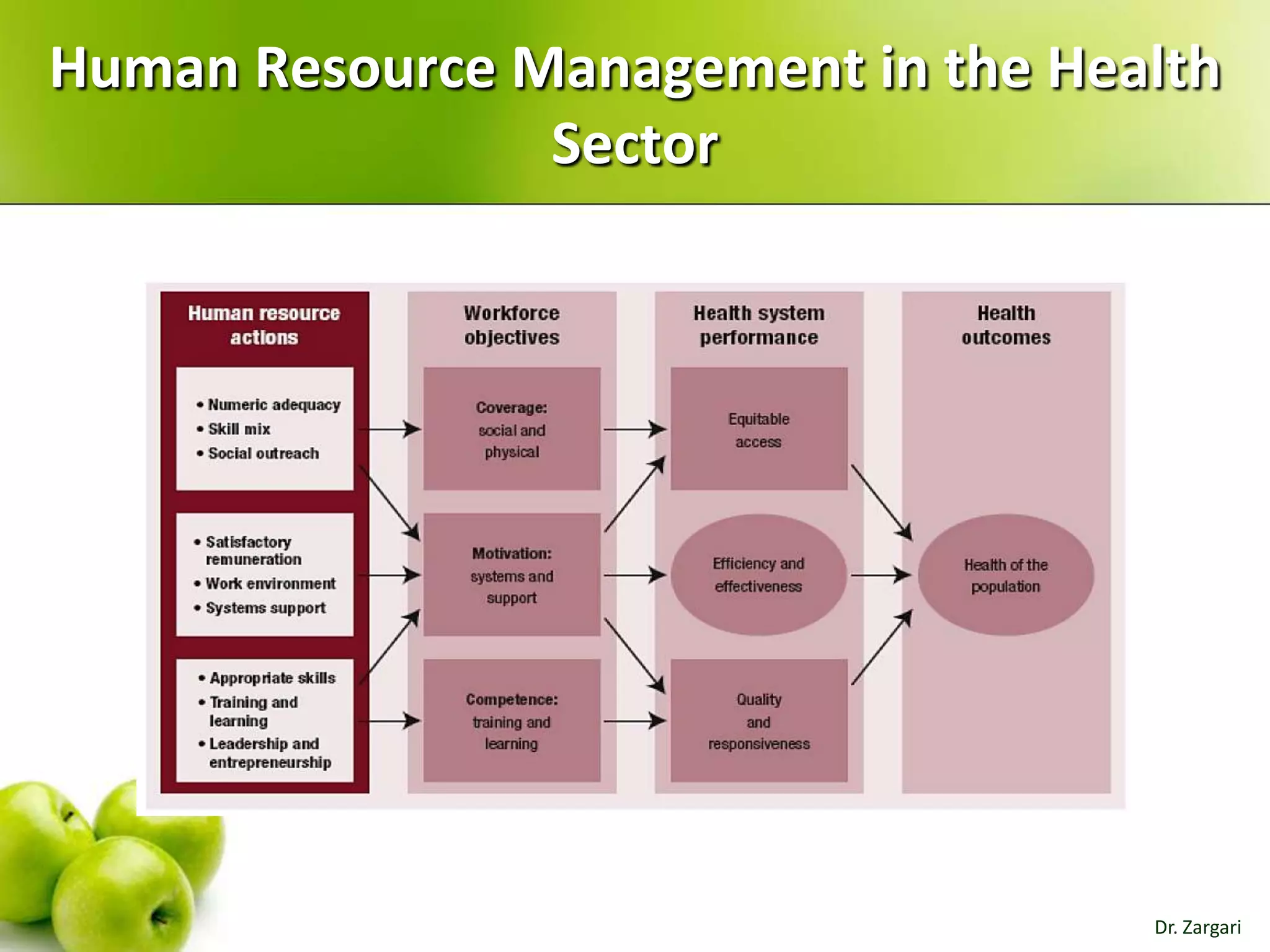
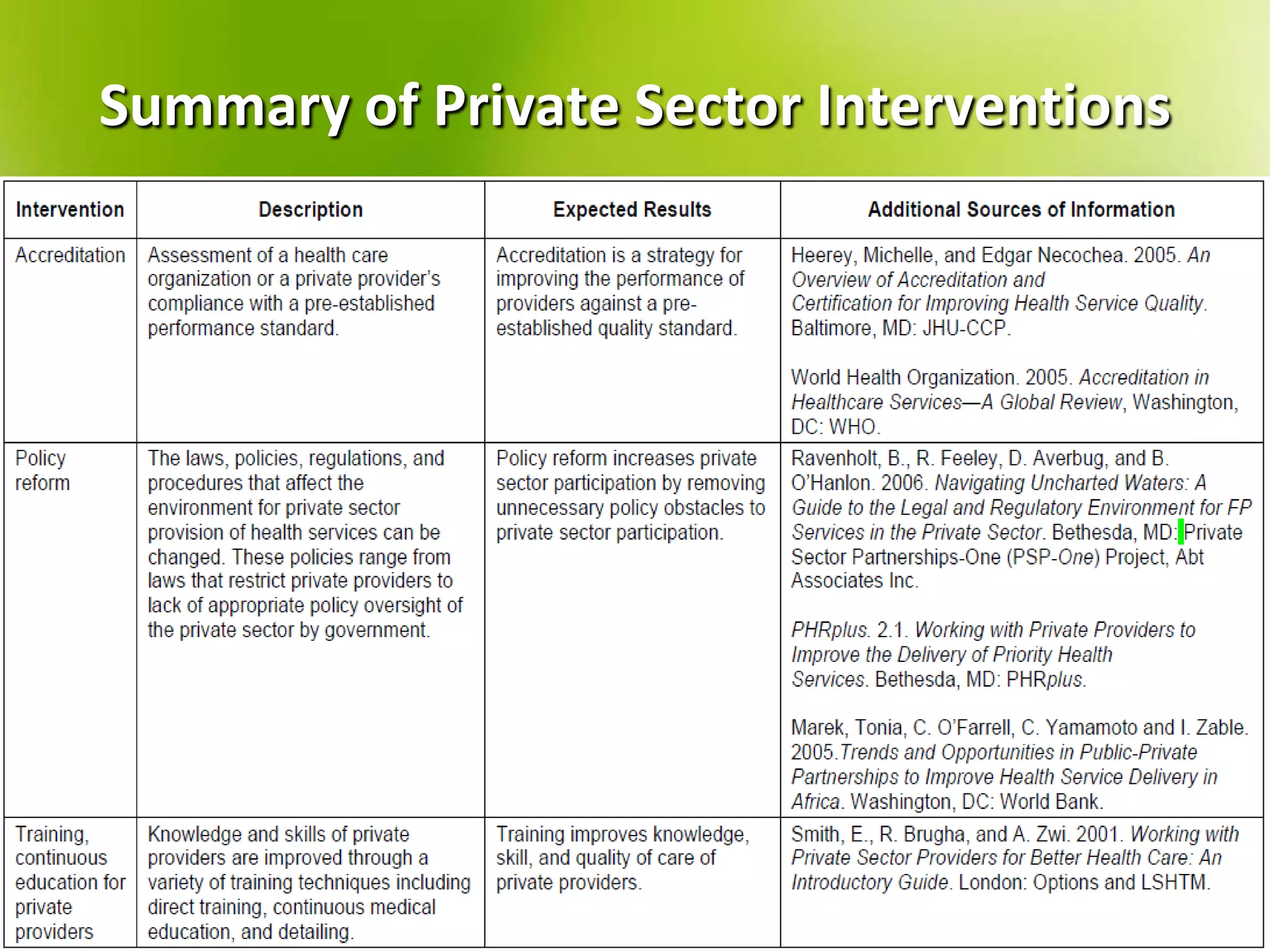
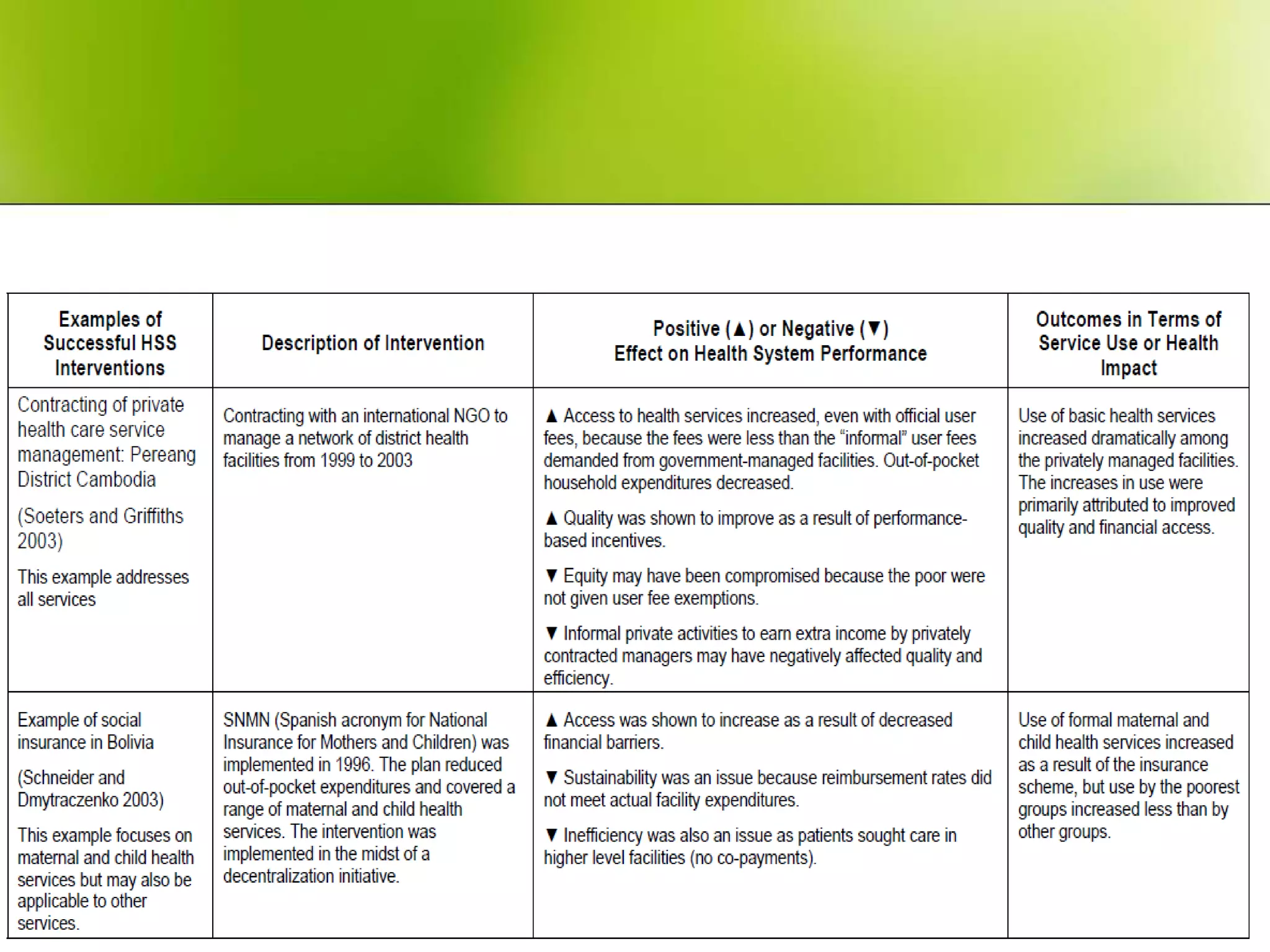
The document provides a comprehensive overview of health systems, emphasizing their definition, key functions, and the importance of stewardship and governance in enhancing health outcomes. It discusses various aspects of health financing, including public and private sources, equity, access, efficiency, and sustainability, highlighting the challenges and strategies related to resource allocation and health service delivery. Overall, the effectiveness of health systems is linked to sound governmental policies that prioritize health equity and performance.