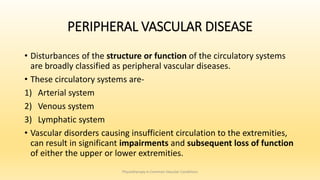
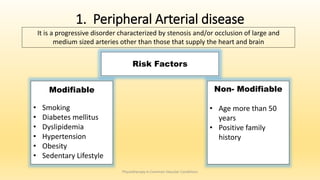
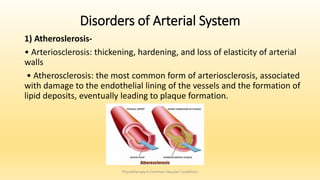
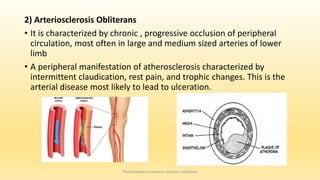
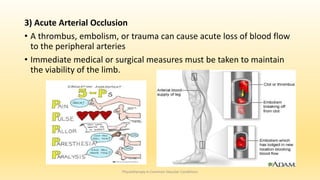
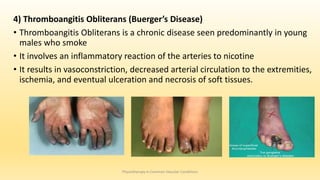
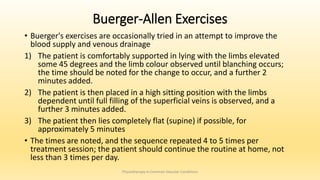
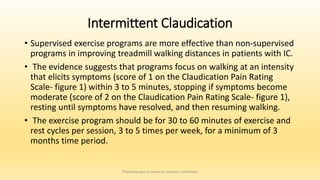
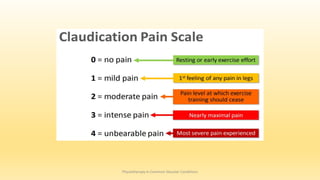
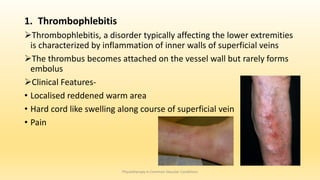
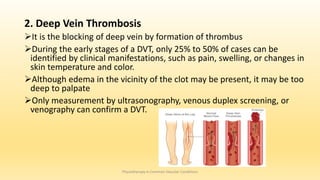
This document discusses physiotherapy approaches in common vascular conditions, particularly focusing on peripheral vascular diseases affecting arterial, venous, and lymphatic systems. It outlines various arterial disorders, their risk factors, clinical manifestations, assessment methods, management strategies, and recent advances in treatment, highlighting the importance of exercise therapy and patient education for effective management. The document also includes findings from recent studies on the effectiveness of warm whirlpool therapy and supervised exercise programs for improving outcomes in patients with peripheral arterial insufficiency.