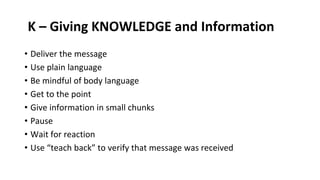
The document discusses the complexities and techniques involved in breaking bad news to patients, highlighting the emotional challenges faced by both patients and physicians. It emphasizes the importance of patient-centered communication and various protocols like the SPIKES approach for delivering difficult information. The text also stresses that proper training can enhance the physician's ability to provide support and maintain patient trust during these critical conversations.


![WHAT IS BAD NEWS?
• ‘Situations where there is either a feeling of no hope, a threat to
person’s mental or physical wellbeing, risk of upsetting an established
lifestyle, or where a message is given which conveys to an individual
fewer choices in his or her life.’ Bor et al., 1993
• ‘...any information which adversely and seriously affects an
individual’s view of his or her future’. Buckman, 1992
• ‘...any information that is not welcome’. Arber and Gallagher, 2003
• ‘...[an] uncomfortable experience for both the giver and the receiver’.
Aitini and Aleotti, 2006.](https://image.slidesharecdn.com/breakingbadnews-231028164039-05cff7ae/85/Breaking-Bad-News-pptx-4-320.jpg)