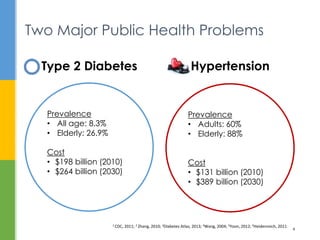
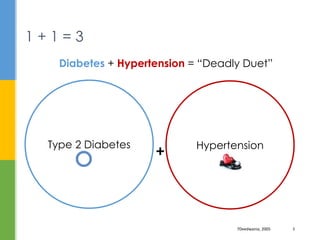
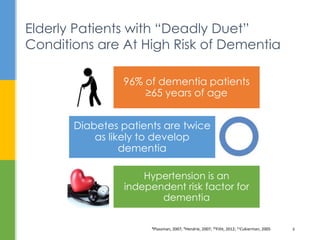
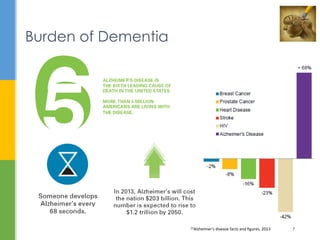
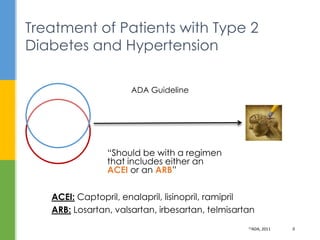
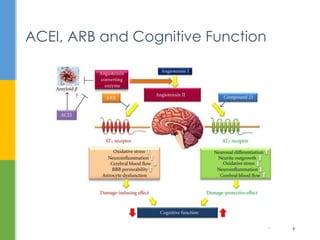
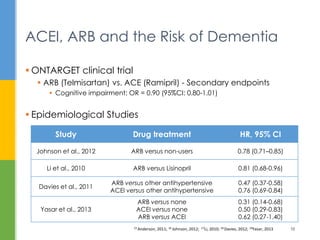
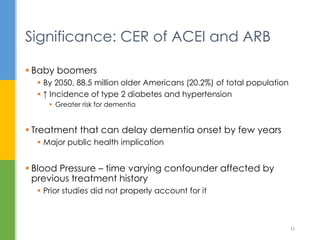
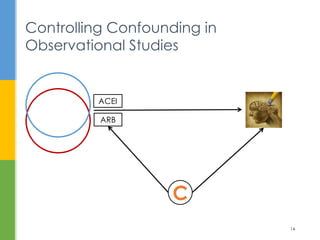
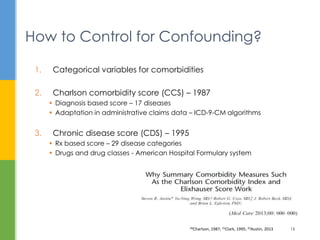
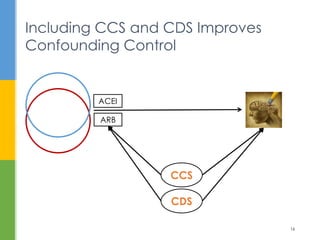
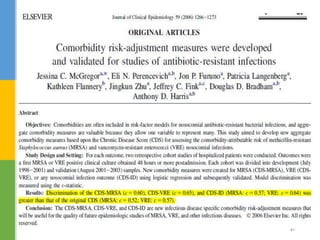
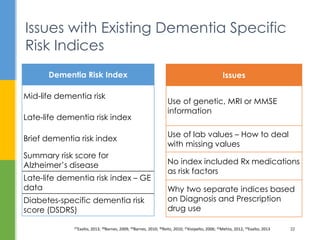
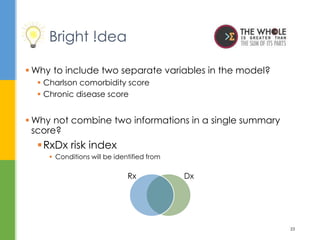
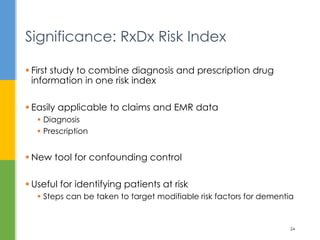
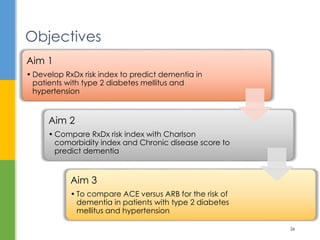
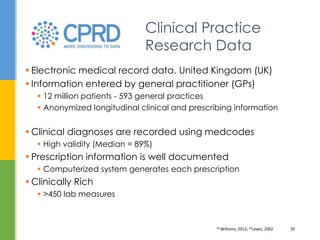
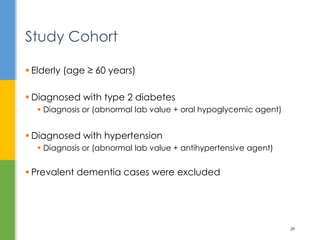
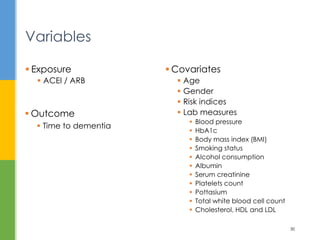
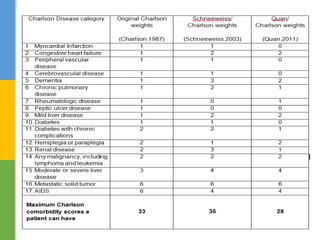
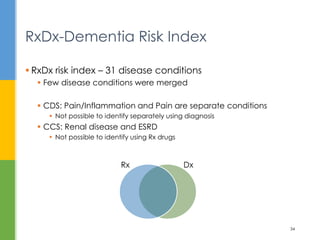
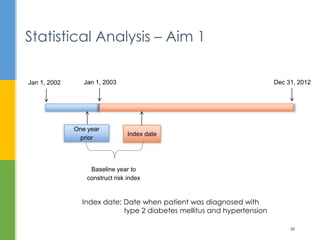
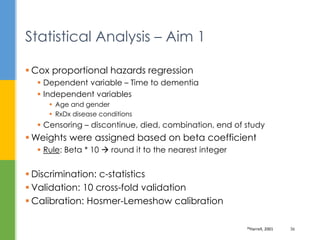
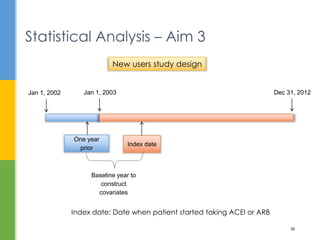
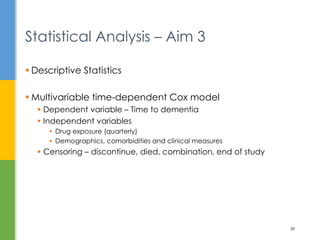
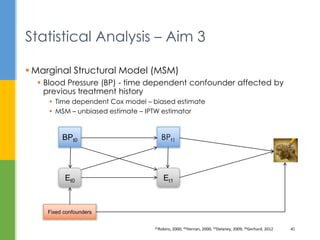
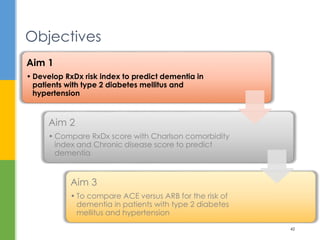
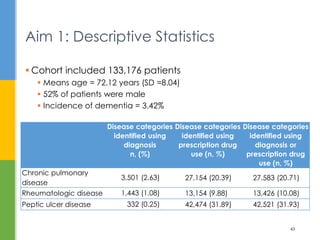
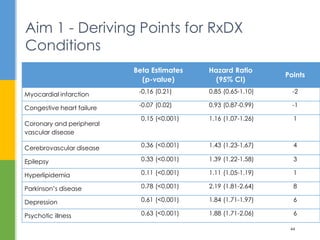
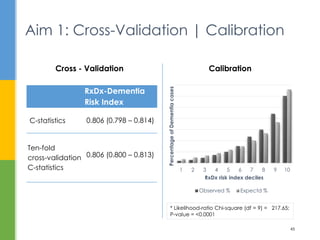
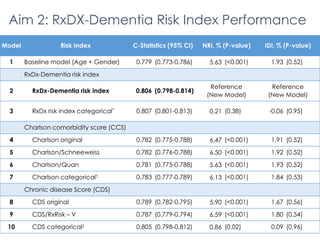
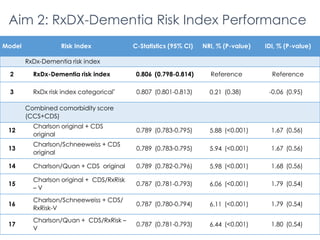
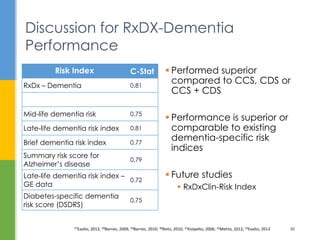
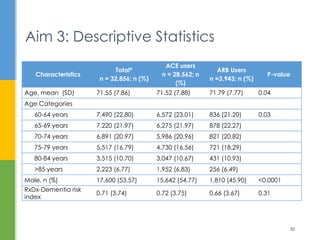
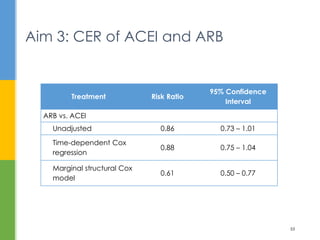
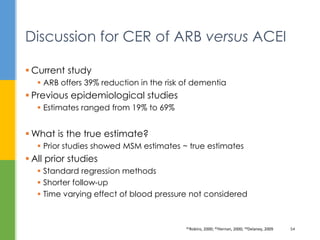
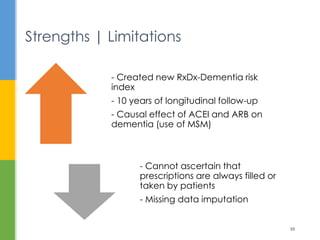
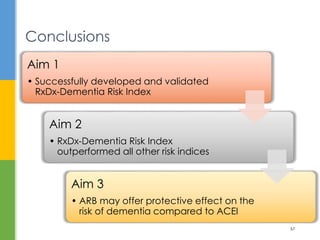
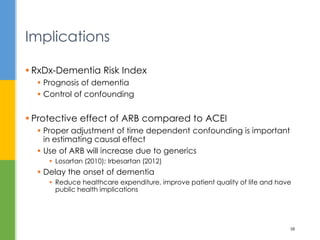
The document examines the comparative effectiveness of ACE inhibitors (ACEI) and angiotensin receptor blockers (ARB) in reducing the risk of dementia in elderly patients with type 2 diabetes and hypertension. It presents a newly developed RXDX risk index aimed at predicting dementia, alongside a comparison of existing comorbidity indices. The study highlights the importance of proper confounding control and provides a methodological framework for future research into dementia risk factors.