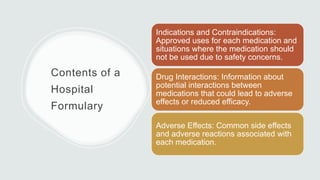
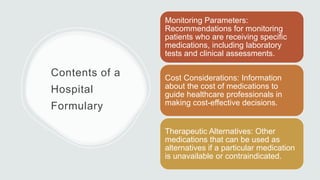
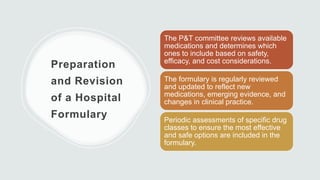
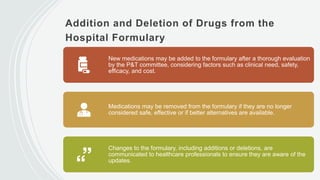
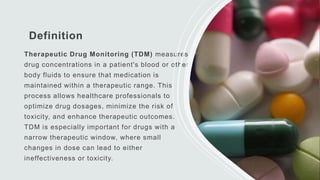
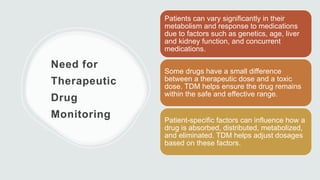
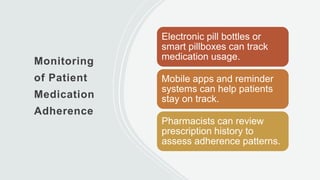
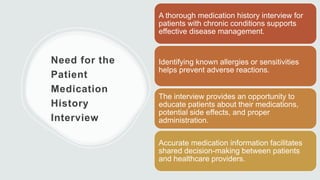
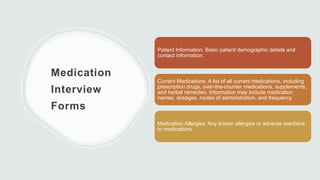
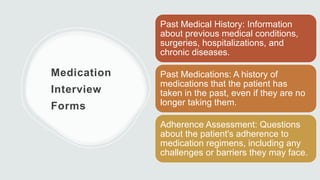
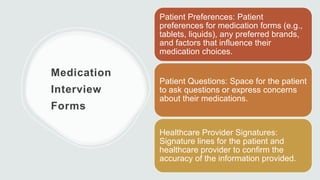
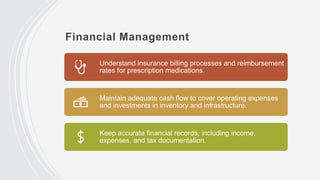
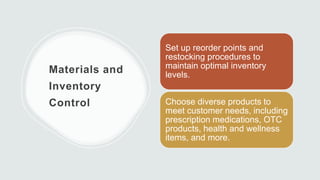
The document outlines the comprehensive drug distribution system in hospitals, detailing the processes from medication order entry to dispensing and administration. It emphasizes the roles of pharmacists, the importance of patient safety through barcoding, and medication reconciliation to ensure accuracy. Additionally, it covers aspects of patient education, billing policies, therapeutic drug monitoring, and the need for adherence to medication regimens, while distinguishing between different drug distribution systems and formulary management.