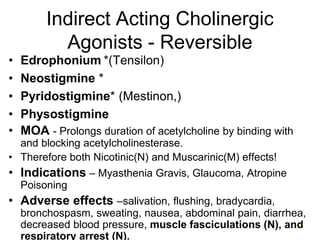
This document provides an overview of the pharmacology of the autonomic nervous system. It discusses cholinergic pharmacology, including direct-acting muscarinic and nicotinic agonists, indirect-acting anticholinesterases, and their therapeutic uses and adverse effects. It also covers adrenergic pharmacology, listing adrenergic receptor subtypes and discussing direct-acting alpha and beta agonists, indirect agonists, and their clinical applications. Finally, it outlines sympathomimetic and sympathomolytic drugs, including ganglionic blockers, alpha and beta blockers, and their mechanisms and side effect profiles.