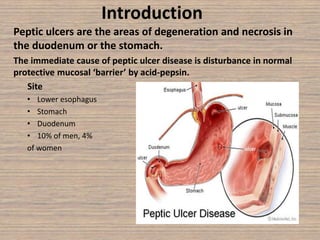
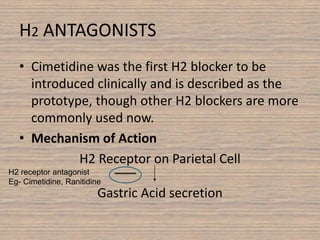
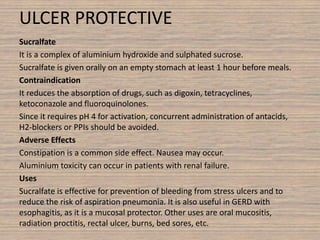
Peptic ulcer disease is caused by a disturbance in the mucosal barrier that protects the stomach and duodenum from acid and pepsin. This allows acid and pepsin to damage the lining and cause ulcers. Treatment involves reducing acid production through proton pump inhibitors or H2 blockers. Additional treatments include antacids to neutralize acid, ulcer protectives like sucralfate to form a protective barrier, and multi-drug regimens to eliminate the bacteria H. pylori when present. Lifestyle changes and avoidance of NSAIDs and smoking are also important parts of treatment and management.