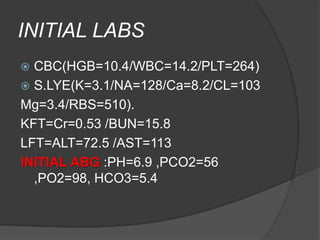
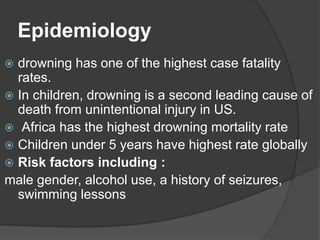
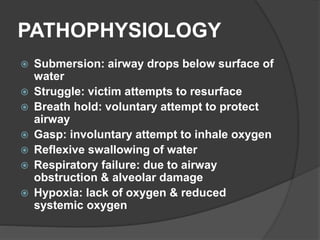
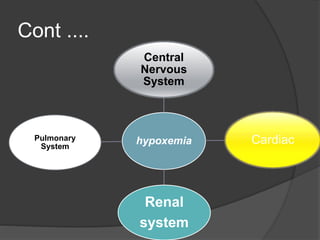
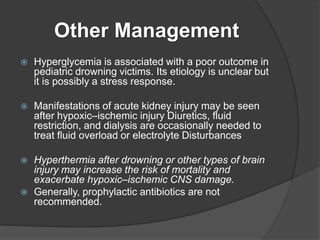
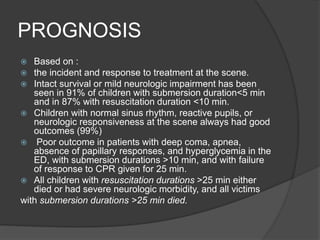
This document describes the case of a 5-year-old male who was found submerged in dirty water for an unknown period of time. He arrived at the emergency room in cardiac arrest and CPR was performed. He was stabilized and transferred to the PICU. Over several days, he was treated with medications, monitored closely, and showed gradual neurological improvement. Drowning is a leading cause of death in children. Prognosis depends on factors like submersion time and response to resuscitation. Prevention through supervision near water is the most effective approach.