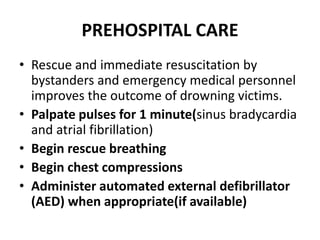
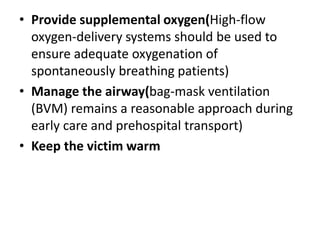
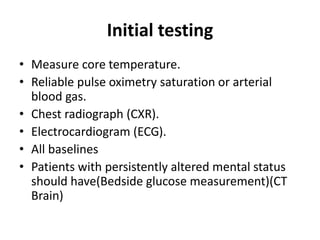
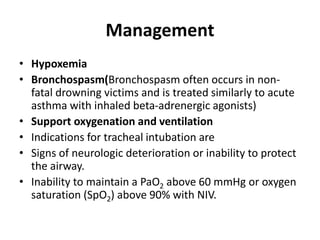
Drowning is a leading cause of accidental death in children worldwide. It occurs most commonly in males ages 1-5 years due to inadequate supervision near bodies of water. Drowning causes hypoxemia which quickly leads to respiratory and cardiac arrest. Survivors can have long-term pulmonary, neurological, cardiovascular and other injuries. Prompt rescue and resuscitation efforts on scene improve outcomes. In the hospital, management focuses on rewarming, correcting hypothermia, hypoxemia and other physiological derangements to prevent secondary neurological injury.