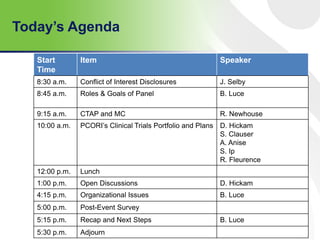
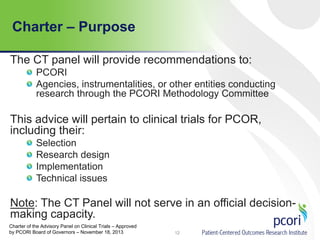
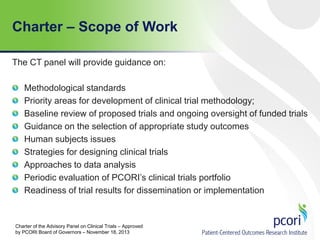
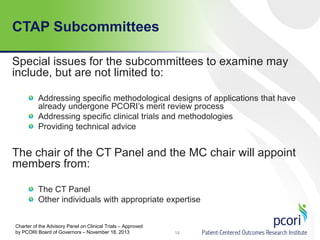
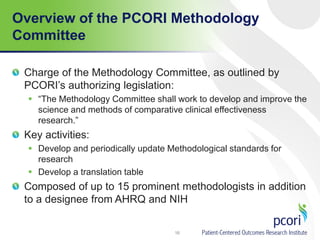
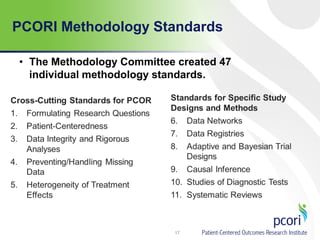
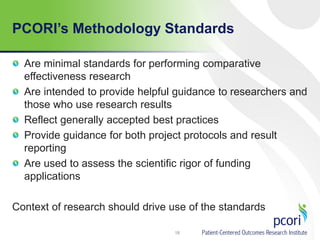
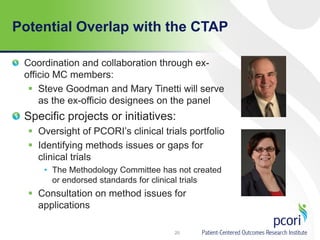
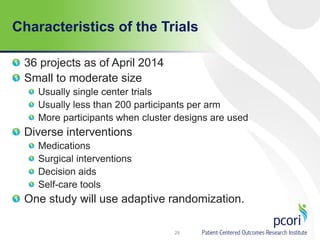
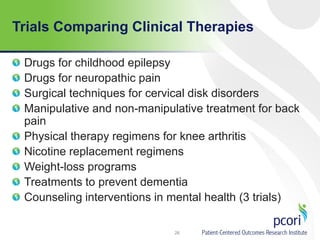
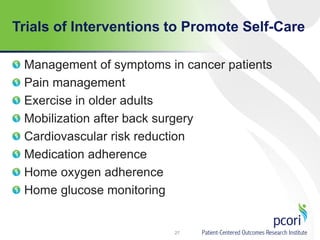
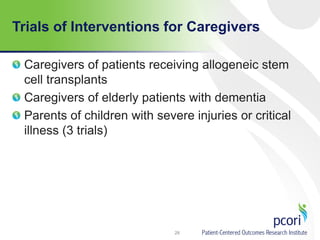
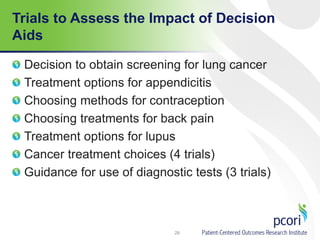
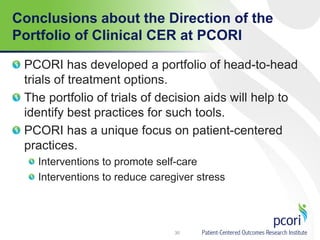
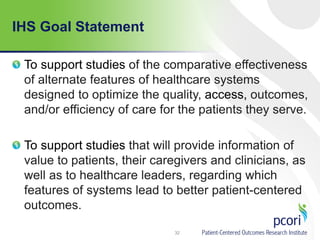
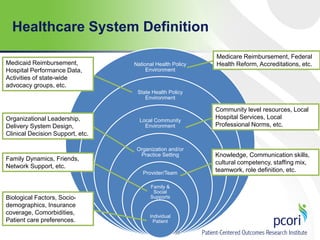
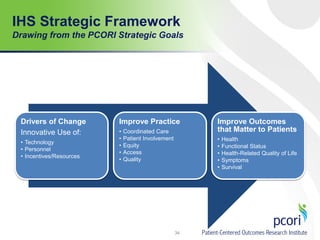
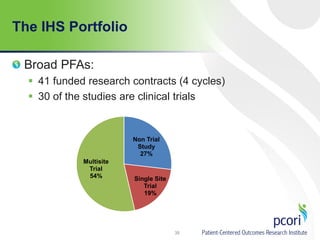
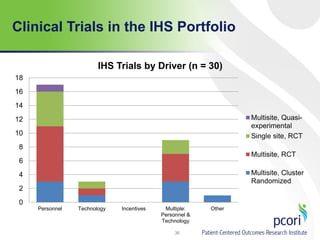
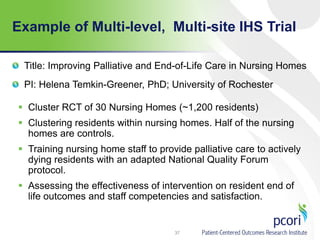
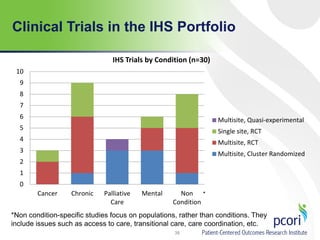
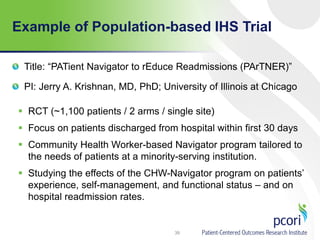
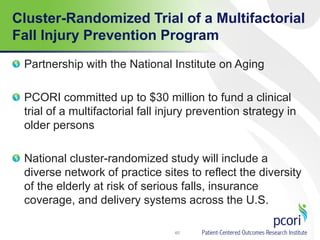
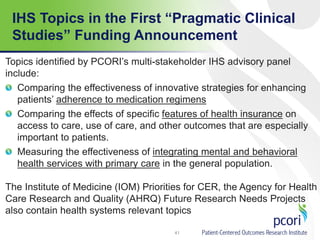
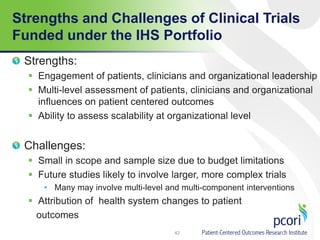
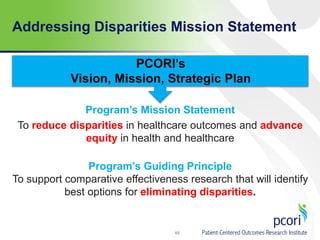
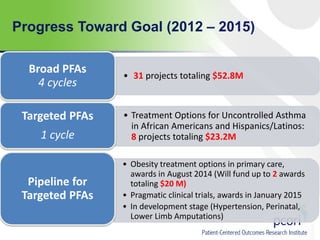
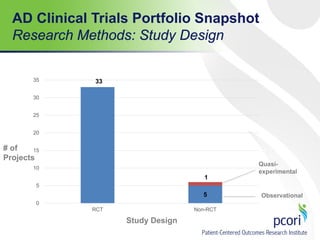
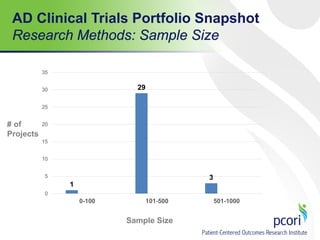
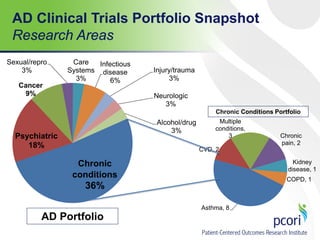
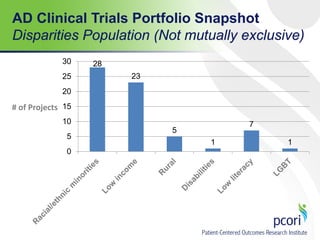
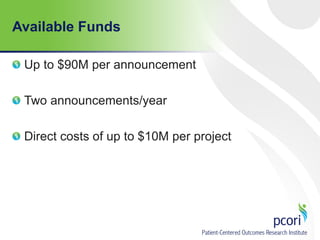
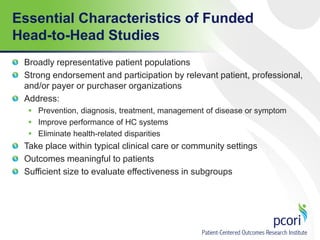
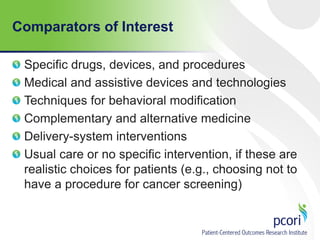
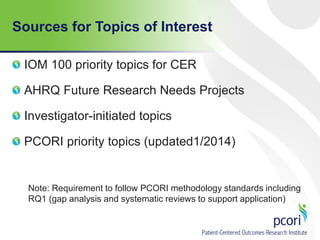
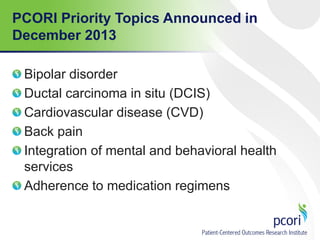
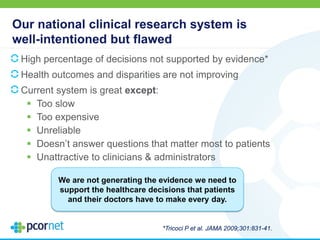
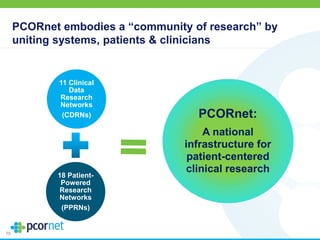
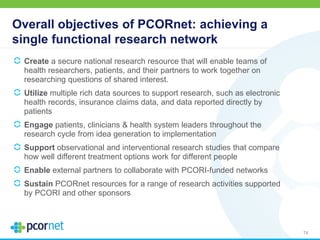
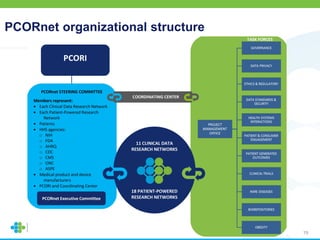
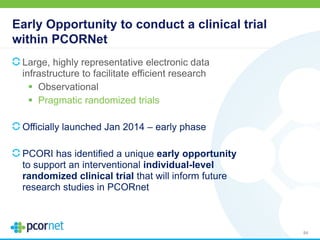
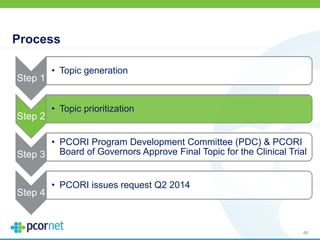
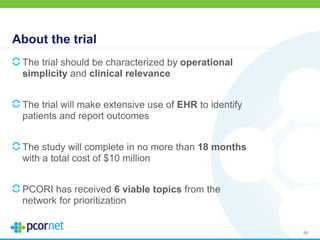
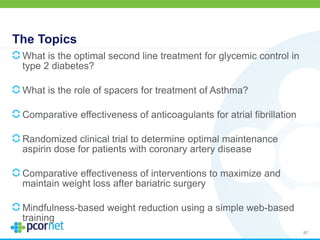
The spring 2014 meeting of the Advisory Panel on Clinical Trials focused on introducing PCORI staff, clarifying panel roles, and discussing the clinical trials research portfolio. The panel is aimed at providing recommendations and guidance on methodological standards and priorities for clinical trial methodologies while ensuring transparency regarding conflicts of interest. Key discussions included various ongoing clinical trials and initiatives aimed at improving healthcare systems and addressing disparities in healthcare outcomes.