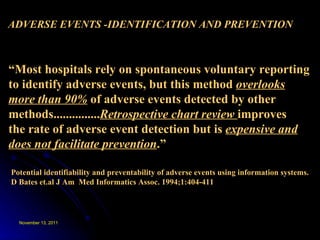
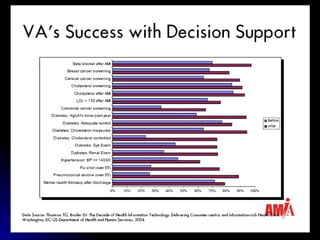
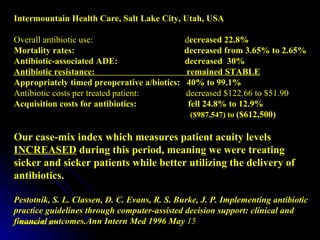
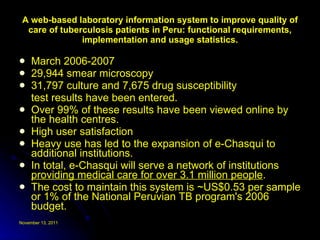
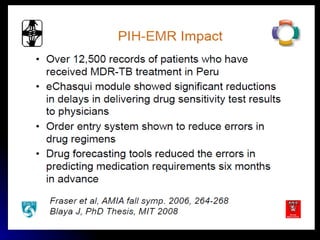
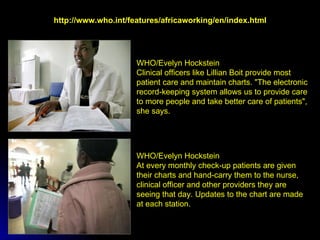
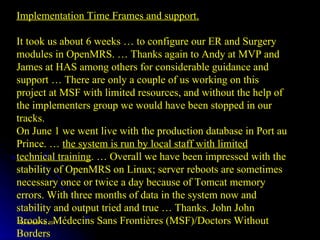
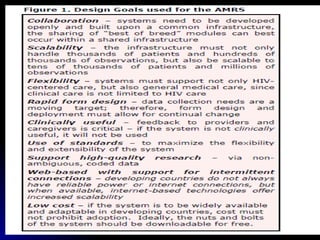
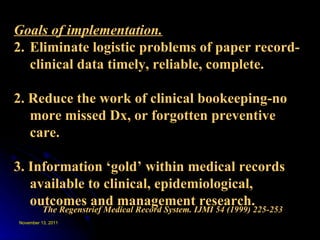
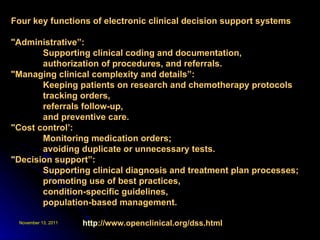
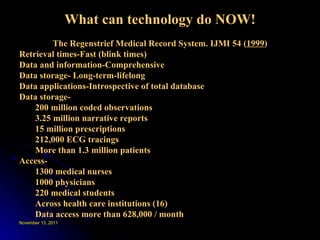
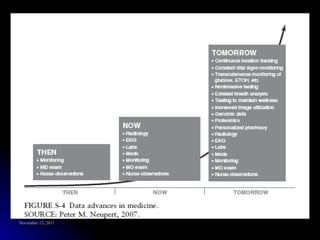
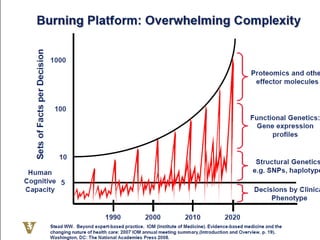
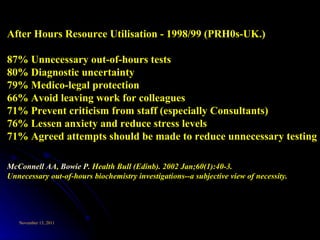
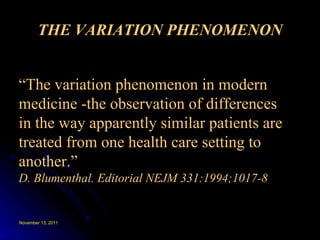
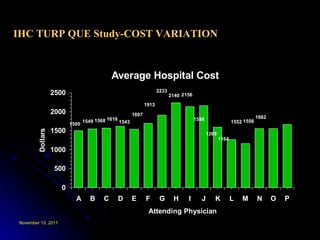
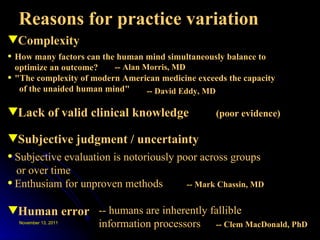
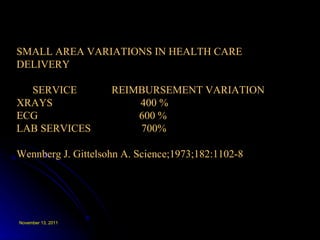
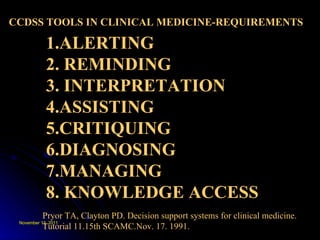
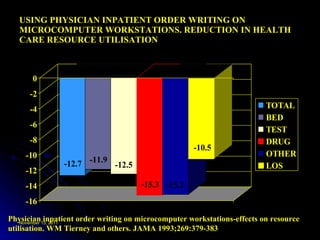
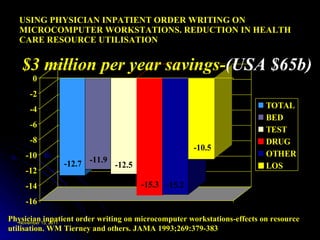
This document discusses the importance of electronic health records and clinical decision support systems for improving healthcare quality and reducing costs and errors. It notes that healthcare information is essential for providing and managing patient care. Clinical decision support systems can help ensure best practices are followed and reduce unnecessary tests and costs. However, the document also finds that healthcare practices still vary greatly between regions and clinicians due to complexity, uncertainty and lack of evidence. More high-quality data and decision support are needed to address these issues and improve consistent high-value care.
![Clinical computing 1976-2011. Current/Future data demands on CDM Technology of clinical computing . Storage, interoperability and standards, forms, data capture, CPOE. Translocating health information technologies MMRS-AMPATH-OpenMRS. Effective CDS tools (MSAccess) show how HIT and CDS works. Meeting the needs of scalability. Role of the internet, WWW, m-Health to meet the demands of modern health care. [VIDEOS]](https://image.slidesharecdn.com/paviawspoctober2011-111112234146-phpapp02/85/Pavia-wsp-october-2011-2-320.jpg)



![High Tech – High Touch-Personal Computing Foreign or Familiar territory? Age Gender Previous computer experience -NOT factors in usage [W.Slack 1976 and 2010]](https://image.slidesharecdn.com/paviawspoctober2011-111112234146-phpapp02/85/Pavia-wsp-october-2011-45-320.jpg)