Paraquat poisoning results from ingestion of the herbicide paraquat. It causes multi-organ damage through generation of reactive oxygen species. Clinical features include mouth ulcers, renal failure, liver damage, and pulmonary fibrosis. Diagnosis is confirmed by urine or blood tests detecting paraquat. Management focuses on decontamination, supportive care, and immunosuppression to reduce lung fibrosis. Prognosis is poor, even with treatment, due to progressive pulmonary damage.
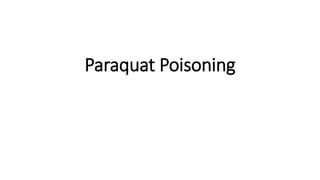





































![Study Description Treatment Mortality
Addo & Poon-King [84] Uncontrolled 72
patients
CP, Dex, MP, vitamin B,
vitamin C
28%
Afzali & Gholyaf [87] RCT 20 patients CP, Dex, MP vs. conventional
treatment
33% vs. 81%
Perriens et al. [89] Uncontrolled 47 patients CP, Dex vs. conventional treatment 63% vs 61%
Lin et al. [86] RCT 23 patients CP, Dex, MP vs. conventional
treatment
31% vs 86%
Lin et al. [80] RCT 50 patients CP, Dex, MP vs. conventional
treatment
68% vs 82%
Lin et al. [85] 16 patients 17 historic
controls
CP, Dex, MP 25% vs 70%
Yasaka et al. [28] Uncontrolled 9 patients Vitamin E 100–4000 mg/day 78%
Hong et al. [99] Uncontrolled 5 patients Vitamin C escalating doses 0%](https://image.slidesharecdn.com/paraquattoxicityexplained-230603002232-7e7dfadc/85/Paraquat-toxicity-explained-pptx-39-320.jpg)





