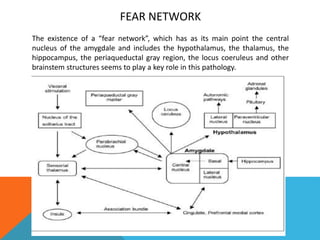
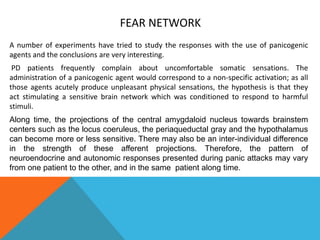
Yiannis Sotiralis presents his experience with panic attacks and shares his understanding of the neurobiology of panic disorder. He was diagnosed with panic attacks 40 days ago when he experienced chest pain, arm burning, and a racing heart at work. Tests showed he did not have a heart condition. His doctor said it was a panic attack. He discusses how panic disorder involves sudden feelings of terror from psychosomatic reactions in the brain's fear circuitry. The amygdala and other brain regions like the hypothalamus and hippocampus are involved in the fear network associated with panic attacks. Understanding the neurobiology helped him gain control over his situation and he has not had an attack in 15 days.
![REFERENCES
Neurobiology of panic and pH chemosensation in the brain John A. Wemmie, MD, PhD
www.dialogues-cns.org
The psychodynamic of panic attacks: a useful integration of psychoanalysis and
neuroscience. De Masi F. Int J Psychoanal. 2004 Apr;85(Pt 2):311-36.
Neuropsychological impairments in panic disorder: A systematic review.
O׳Sullivan K1, Newman EF2. J Affect Disord. 2014 Jun 18;167C:268-284. doi:
10.1016/j.jad.2014.06.024. [Epub ahead of print]](https://image.slidesharecdn.com/panicattack-140709142535-phpapp02/85/Panic-attack-8-320.jpg)