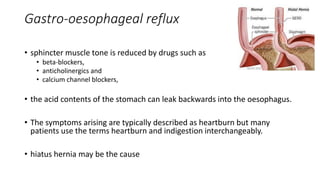
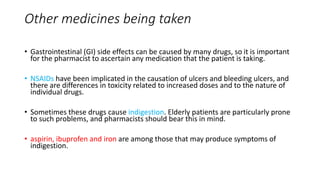
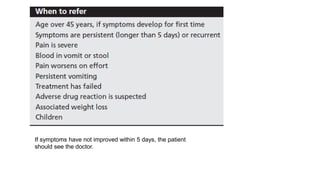
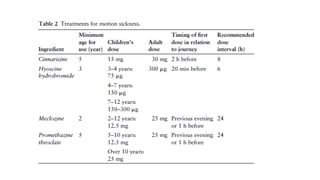
This document discusses gastrointestinal tract problems like indigestion, nausea, and vomiting. It provides details on symptoms, risk factors, management, and conditions that may present as indigestion but require referral like ulcers, gallstones, GERD, IBS, and atypical angina. Motion sickness prevention is also addressed, noting the importance of selecting a prophylactic treatment based on a patient's age and details of their upcoming travel.