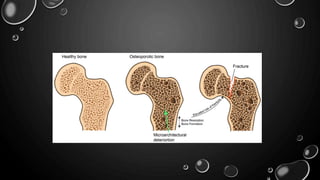
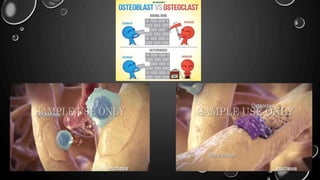
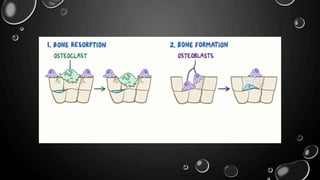
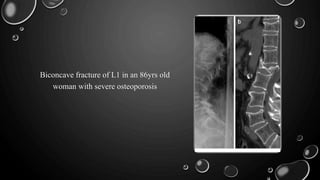
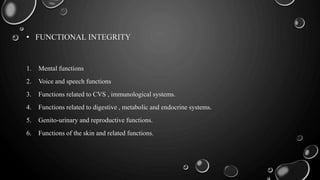
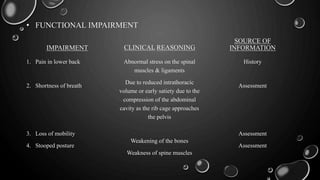
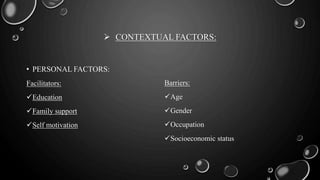
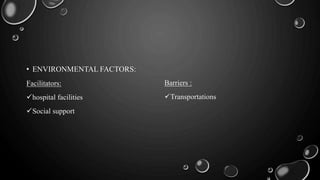
The document outlines osteoporosis, a condition characterized by reduced bone density leading to increased fracture risk and pain. It discusses its pathophysiology, types (primary and secondary), causes, clinical features, diagnostic methods, and the impact of various contextual factors on individuals affected by the disease. Osteoporosis becomes particularly common post-menopause and can be influenced by dietary, lifestyle, and genetic factors.