Osteomyelitis march 2018
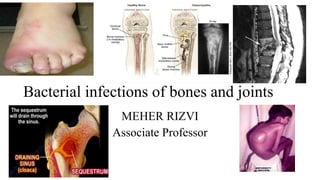
- 1. Bacterial infections of bones and joints MEHER RIZVI Associate Professor
- 2. Objectives 1. Name the bacteria which most commonly cause osteomyelitis and septic arthritis in adults and children 2. List various routes by which bacteria gain access to bones and joints 3. Describe the pathogenesis of osteomyelitis and septic arthritis 4. Describe the procedures used for establishing laboratory diagnosis of bone and joint infections
- 3. • Osteomyelitis: Inflammation of bone and bone marrow due to bacterial infection • Acute osteomyelitis: 1 in 5000 children • Chronic osteomyelitis: 2 in 10,000 adults • Childhood osteomyelitis: long bones of the legs and upper arms. • Adults osteomyelitis: bones of the vertebrae. • Types of osteomyelitis: • Post traumatic osteomyelitis: (47% cases) • Osteomyelitis due to vascular insufficiency: (34% cases) • Osteomyelitis due to hematogenous spread: (19%) • Osteomyelitis post infection of prosthetic joints
- 4. Pathogenesis • Bone is normally resistant to bacterial colonization • Bacteria form a biofilm in the metaphysis (primary focus) • Biofilms protect bacteria from host immune response • Abscess in metaphysis • Subperiosteal abscess • Sequestrum formation (bone death) • Involucrum formation (New brittle bone formation) • Pus perforates periosteum and forms abscess in soft tissues • Abscess bursts on surface and forms discharging sinus
- 5. Factors affecting pathogenesis • Virulence of the infecting organism • Underlying disease • Immune status of the host • Type, location and vascularity of the bone. Factors that compromise bone integrity: • Trauma • Surgery • Presence of foreign bodies • Placement of prostheses Leads to the onset of bone infection
- 6. • Signs & Symptoms • Fever, chills, irritability, fatigue. • Tenderness, redness, and warmth in the area of the infection. • Swelling around the affected bone. • Lost range of motion. • The symptoms for acute and chronic osteomyelitis are very similar
- 7. Factors leading to chronic osteomyelitis Trauma Diabetes Prosthetic orthopaedic device Peripheral vascular disease Chronic joint pain i/v drug abuse Immunosuppression Alcoholism
- 8. Hematogenous osteomyelitis • Primary hematogenous osteomyelitis: Most common in infants and children • Site: long bone metaphysis. • Sinus tracts may form if infection extends into soft tissue. • Secondary hematogenous osteomyelitis: • Occurs when childhood infection is reactivated. • Adults: • Vertebrae: most common, followed by long bones, pelvis, clavicle • Infections recur and present with minimal constitutional symptoms and pain.
- 9. Haematogenous osteomyelitis of tubular bone in child Blood flow is slow and turbulent and predisposes to bacterial seeding. Lining cells have little or no phagocytic activity
- 10. Etiology Most common: • Staphylococcus aureus • Pseudomonas aeruginosa • Enterobacteriaceae • Less common organisms: • anaerobe gram-negative bacilli.
- 11. • Infants • Children • Adults Streptococcus agalactiae (Group B Streptococci) Staphylococcus aureus Escherichia coli Staphylococcus aureus Streptococcus pyogenes (Group A Streptococci) Streptococcus pneumoniae Haemophilus influenzae CA-MRSA Staphylococcus aureus Staphylococcus epidermidis Pseudomonas aeruginosa Escherichia coli
- 12. Etiology associated with certain risk factors: • Penetrating wound, open fracture: Staphylococcus aureus • In dwelling prosthetic device: Staphylococcus epidermidis • Intravenous drug users: Pseudomonal infections. • Gastrointestinal or genitourinary infections: Escherichia coli & others • Tooth abscess, gingival disease, dental extraction: Streptococcus viridans • Mycobacterium tuberculosis: Bone tuberculosis • Sickle cell disease: Salmonella species in the West Staphylococcus aureus in Middle East &Africa
- 13. Acute hematogenous osteomyelitis • Symptoms of a severely acute illness. The child is irritable and restless. • Headache, high-grade fever with chills, tachycardia occurs. • The affected limb is held in semiflexion, surrounding muscles are in spasm due to excruciating pain. • On examination patient resists the passive movement of the affected limb due to muscle spasm. • The affected site is tender to deep palpation. • Initially, swelling is not present but within a few days the soft tissues about the affected site become edematous and red, indicating subperiosteal abscess formation.
- 15. Vertebral osteomyelitis: haematogenous origin • Source of infection: skin, soft tissue, respiratory tract, genitourinary tract, infected intravenous sites, and dental infections. • Complaints: slow progression- 3 weeks to 3 months. • Localized pain, swelling and tenderness of the involved vertebrae • Weakness of the vertebral column and surrounding muscles • Difficulty transitioning from a standing to a sitting position
- 16. Osteomyelitis in children with sickle cell disease • Osteomyelitis is the second most common infection in SCD • Common organisms: • Salmonella species (Most common in America & Europe) • S aureus (Most common in Middle East) • Serratia species • Proteus mirabilis.
- 17. Contiguous-focus and posttraumatic osteomyelitis: Adults Common etiology Staphylococcus aureus Staphylococcus epidermidis Gram negative bacilli Anaerobes Nocardia- rare
- 18. Contiguous-focus and posttraumatic osteomyelitis: Adults Direct inoculation of bacteria: • Trauma • surgical reduction • internal fixation of fractures • prosthetic devices Can spread from: • soft-tissue infection • septic arthritis • nosocomial infection Vascular compromise: Diabetes • Infection begins outside the bony cortex and moves in toward the medullary canal: Contrast to hematogenous infection • Low-grade fever, drainage, and pain. • Most common site: Tibia • Most common etiology: S aureus
- 19. Osteomyelitis in diabetes mellitus • Cause: minor trauma to the feet • Foot ulcers allow bacteria to reach the bone • Poor glycaemic control. Patients may not experience any pain because of peripheral neuropathy Presentation: perforating foot ulcer, cellulitis or an in-grown toenail. • Etiology: multiple organisms • Streptococcus species, • Enterococcus species, • Staphylococcus aureus • Staphylococcus epidermidis • Gram-negative bacilli, • Anaerobic organisms (Bacteroides)
- 20. Skeletal Tuberculosis (Pott’s Disease) •Painful bones •The infected bone will begin to weaken and become curved •Absence of feeling and movement in the diseased bone •Due to the bone being weakened, it has a high risk of being fractured Tubercular osteomyelitis Pyogenic osteomyelitis Longstanding history of months to years History of days to months Presence of active pulmonary tuberculosis Not present Most common location: Thoracic spine Lumbar spine > 3 contiguous vertebral bodies involved Two vertebrae and intervening disc Vertebral collapse : Common (67%) Less common (21%)
- 21. Complications • Bone death (osteonecrosis). An infection can impede blood circulation within the bone, leading to bone death. • Septic arthritis. In some cases, infection within bones can spread into a nearby joint. • Impaired growth. In children, the most common location for osteomyelitis is in the softer areas, called growth plates, at either end of the long bones of the arms and legs. Normal growth may be interrupted in infected bones. • Skin cancer. If osteomyelitis has resulted in an open sore that is draining pus, the surrounding skin is at higher risk of developing squamous cell cancer.
- 22. In a nutshell
- 23. Staphylococcus aureus • Gram positive cocci seen in clusters • Grows on blood agar: beta hemolysis • Golden coloured colonies • Tests: • Catalase positive • Coagulase positive • DNAase positive
- 25. Virulence markers • Protein A • Staphylokinase • DNAase • Panton valentine leucocidin: Important virulence factor in CA-MRSA Forms pores in the membranes of WBCs • Exfoliative toxin • Toxic shock syndrome • Enterotoxins Superantigens
- 27. Antimicrobial resistance: • Penicillin: Drug of choice for Staphylococcus aureus • Plasmid mediated penicillin resistance: Beta lactamase production • Methicillin introduced: Resistant to beta lactamase • Methicillin sensitive Staphylococcus aureus (MSSA) • Alteration of PBP2a (mec A gene): Methicillin resistant Staphylococcus aureus (MRSA). Chromosomal mediated methicillin resistance • Nosocomial MRSA strains (HAMRSA): carried on Staphylococcal cassette chromosome (SCC) type I-III : • Drug of choice: Vancomycin, teicoplanin, • Community acquired MRSA (CAMRSA)- carried on SCC type IV • More virulent (PVL), Less resistant to antibiotics. Sensitive to clindamycin Global antimicrobial resistance 1930s 2020s
- 29. • Vancomycin intermediate Staphylococcus aureus (VISA) • Vancomycin resistant Staphylococcus aureus (VRSA) • Antibiotic options: • Linezolid • Telavancin • Daptomycin • Ceftaroline/Ceftabiprole
- 30. MRSA: Infection control procedures • Personnel with active S. aureus lesions and carriers have to be excluded from patient caring areas • Eradication of MRSA: Topical application of mupirocin to nasal or perineal areas • Patients are screened for MRSA • Contact precautions: Hand hygiene before and after patient contact Wearing gloves, gowns etc
- 33. Pseudomonas aeruginosa Gram negative, motile bacilli, single polar flagella Oxidase positive, Strong aerobe Non fastidious: Grows on Nutrient agar. Can grow at 420C Produces various pigments: pyocyanin, pyoverdin, pyomelanin, pyorubrin CLED: Non lactose fermenting Hugh Leifson test CLED Blood agar Nutrient agar
- 34. Pseudomonas aeruginosa- Ubiquitous saprophytes in nature. • Classical nosocomial pathogen: moist atmosphere of hospitals: • Skin & soft tissue infections • Burn patients: are at risk of septicaemia • Ecthyma gangrenosum: Acute necrotizing condition in HIV/neutropenic individuals • Dermatitis: Papular/vesicular/follicular lesions. Outbreaks in spas/ swimming pools • Bone & joints infections • Septic arthritis Recall: What other infections? Other significant infections • Ventilator associated pneumonia • Chronic respiratory tract infections • Cystic fibrosis • Infective endocarditis in I/V drug abusers
- 35. Virulence markers • Adhesion: Pili/flagella • Exotoxin A • Alginate coat: mucoid strains. Produce biofilms: • Multidrug resistance • Multi disinfectant resistance • Wide temperature range • Intrinsic resistance to some antibiotics. • Antipseudomonal drugs: • Penicillins: Piperacillin, Ticarcillin • Cephalosporins: Ceftazidime, cefoperazone, cefepime • B/BLI: Piperacillin-tazobactam • Aminoglycosides: Amikacin, tobramycin • Fluoroquinolones: ciprofloxacin/ levofloxacin • Carbapenems: imipenem, meropenem • Polymixin Antimicrobial resistance
- 36. Enterococcus spp. • Gram positive cocci seen mostly in pairs. • Non fastidious. Hardy • Catalase negative • Hemolysis: alpha, beta, gamma • Bile aesculin test positive: • Survive extremes of pH, temperature, salinity • Intrinsic resistance: Cephalosporins & cotrimoxazole • Low level intrinsic resistance: Penicillins, aminoglycosides • Penicillin and aminoglycosides • Vancomycin and aminoglycosides Intestinal commensal Synergistic Combination therapy Species Enterococcus faecalis Enterococcus faecium
- 37. Resistance in Enterococcus • High level Aminoglycoside Resistance (HLAR): Synergy ineffective • Vancomycin resistance: Vancomycin resistant enterococci (VRE) • Mediated by Van gene: Van A-E. • Van A displays high level resistance • Alters target site- reduced affinity to vancomycin • Treatment options: quinupristin-dalfopristin, linezolid, daptomycin, tigecycline • Synergistic combination: Ceftaroline & daptomycin D-alanyl-D-alanine side chain of peptidoglycan layer is altered to D-alanyl-D- lactate
- 38. Septic Arthritis: Infection of joint space Complications: • Septicemia • Pre- existing joint disease like rheumatoid arthritis • Extension of osteomyelitis or other infection near the joint • Infection subsequent to intra-articular injection, arthroscopy or orthopaedic surgery- insertion of joint prosthesis
- 39. Clinical features: Generally only one joint involved (knee) Sudden onset Severe pain Fever Swelling and redness of the joint Causative organism : S. aureus most common ( as in osteomyelitis ) N. gonorrhoeae N. meningitidis Ureaplasma urealyticum
- 40. Osteomyelitis: diagnosis Complete medical history Complete general examination Complete physical examination Possible clinical findings • Pain • Fever • Tenderness • Erythema • Swelling • Sinus tract • Limp
- 41. Laboratory diagnosis- Osteomyelitis • Complete blood count • Elevated WBC count/ Raised CRP/ Raised ESR • Bone/tissue biopsy/ Fine needle aspirate: Gold standard • Blood culture: Hematogenous osteomyelitis (60% positivity) • Wound/Pus culture • Fluid aspirate from joint (Suppurative arthritis) • Imaging techniques: CT scan, MRI For confirmation of diagnosis Serology : Brucella Molecular methods : Detection of bacterial DNA in synovial fluid
- 43. Treatment : Initial therapy: Empirical antibiotics High dose parenteral antibiotics 1-2 weeks till fever and symptoms subside Imipenem; piperacillin-tazobactam; a quinolone plus clindamycin; or an extended-spectrum cephalosporin plus clindamycin Specific therapy: 4-6 weeks De-escalate to oral antibiotics after patient clinically stable Follow CRP for guidance on duration of treatment
- 44. Empirical treatment: parenteral M. tuberculosis: Antitubercular drugs Anaerobes: Metronidazole or clindamycin P. aeruginosa : Ciprofloxacin and gentamicin Escherichia coli : Ciprofloxacin , ceftriaxone Streptococci : Penicillin, clindamycin Staphylococcus aureus: Flucloxacillin + gentamicin / clindamycin / fusidic acid
- 45. Surgical intervention • Bone death (osteonecrosis): If small sections of dead bone is infected: bone can heal after surgical removal of small parts of bone. • If a large section of bone is dead: limb surgically removed (amputated) to prevent spread of the infection. • Amputation, limited resection, debridement, and antibiotic therapy alone each have a place in the management of diabetic foot osteomyelitis.
