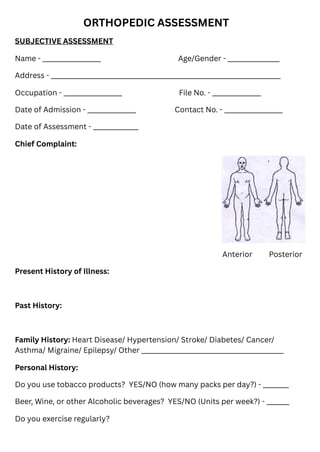
The document is an orthopedic assessment form that collects detailed subjective and objective data from patients, including personal, medical, and pain histories. It includes sections for general examination, sensory and motor evaluation, and specific assessments related to limb function and diagnostic goals. The form is structured to support the establishment of provisional diagnoses and treatment plans.