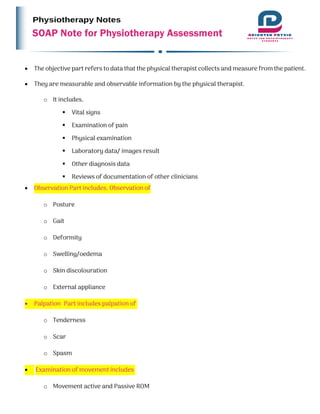
The document outlines the SOAP note method used in physiotherapy assessments, which includes Subjective, Objective, Assessment, and Plan components to evaluate a patient's issues comprehensively. It emphasizes the importance of understanding both patient and clinician perspectives and organizing care effectively. The document details the specific information to be gathered in each section, including vital signs, patient history, and treatment plans.