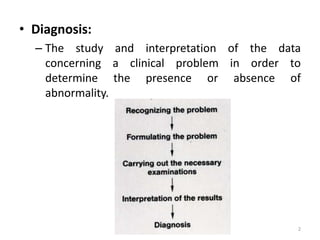
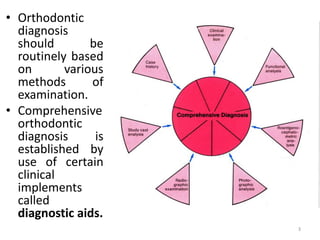
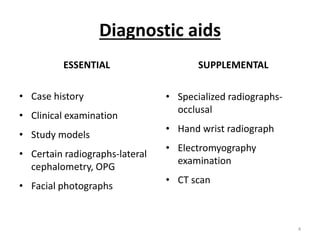
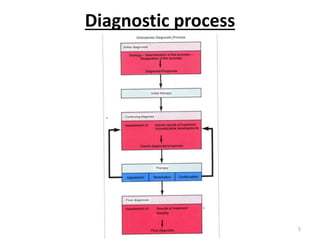
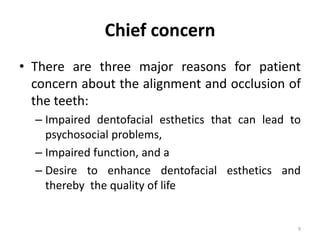
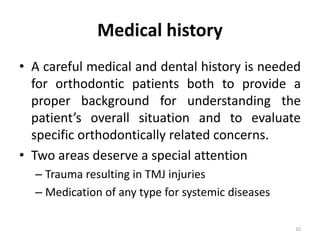
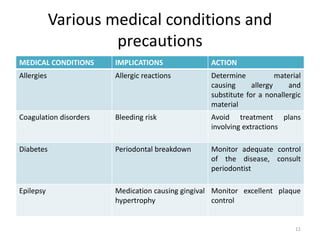
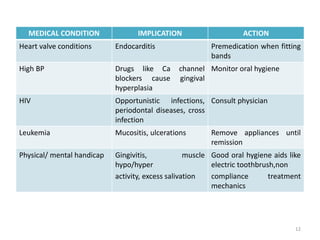
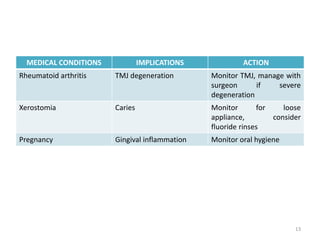
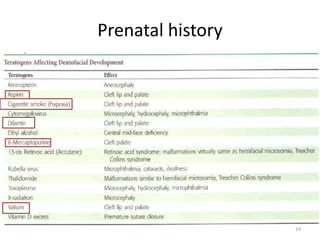
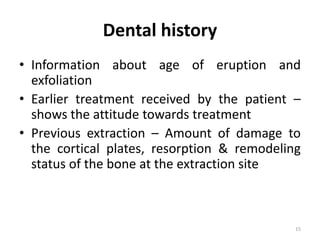
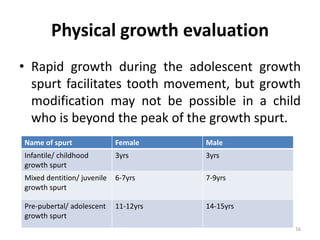
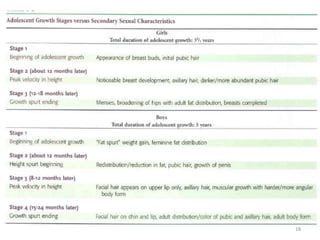
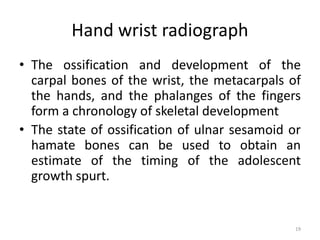
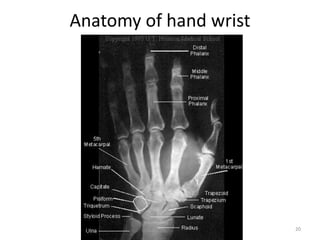
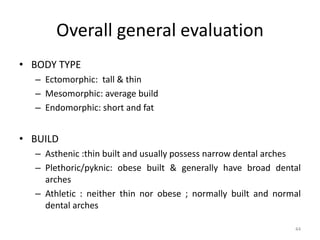
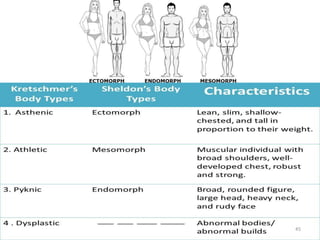
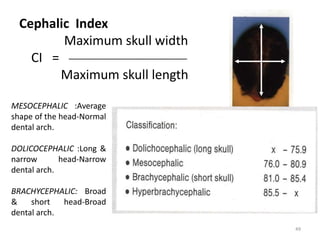
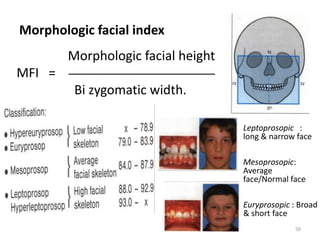
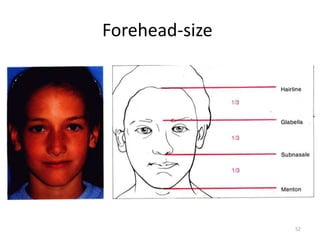
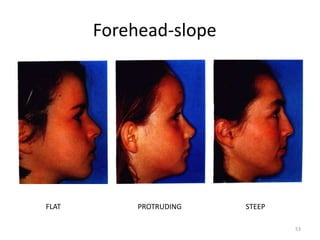
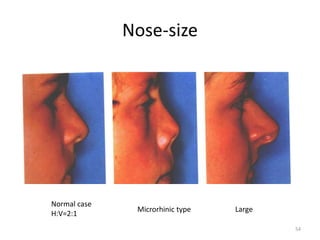
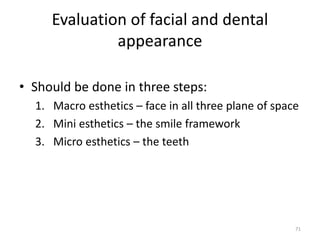
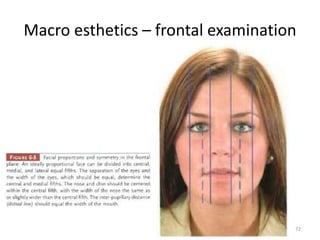
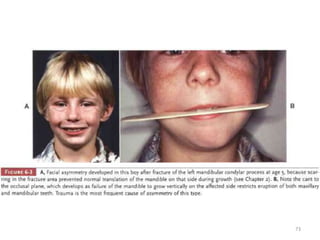
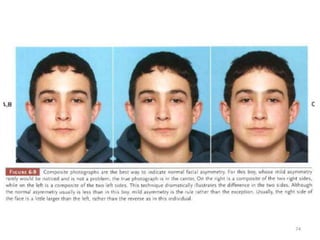
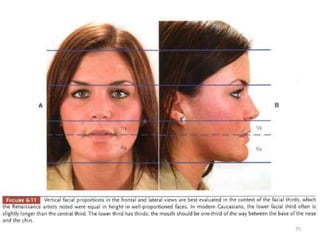
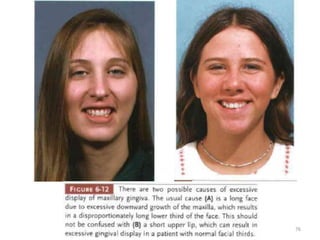
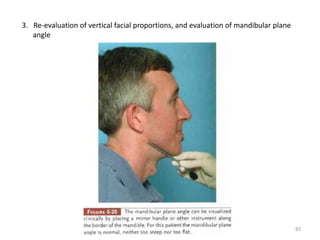
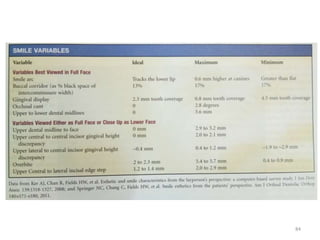
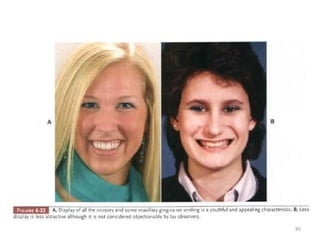
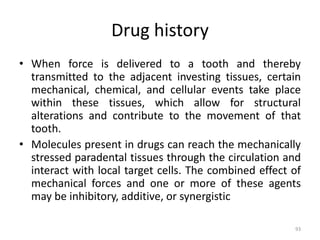
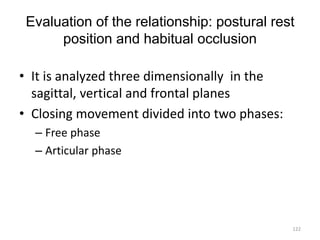
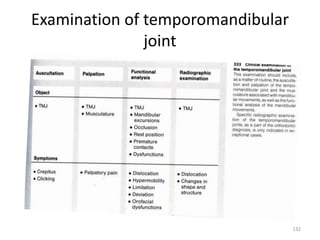
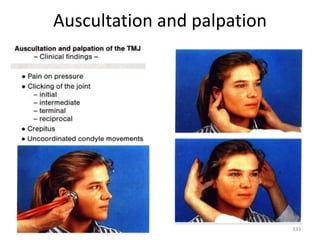
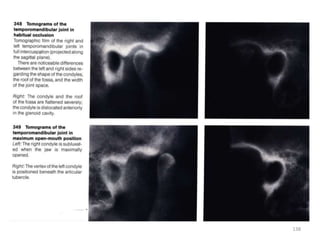
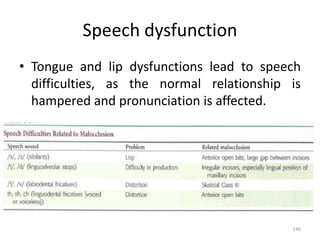
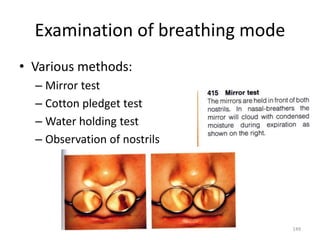
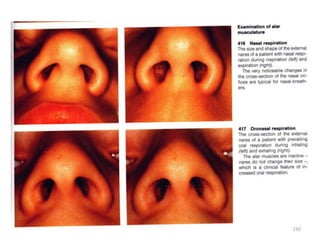
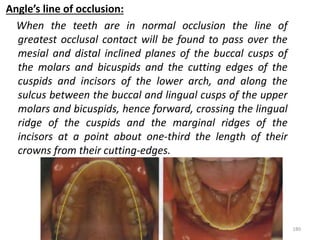
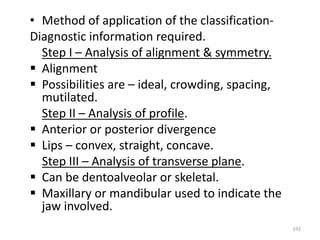
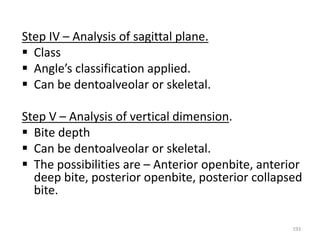
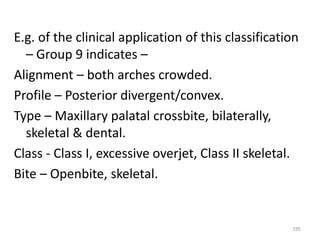
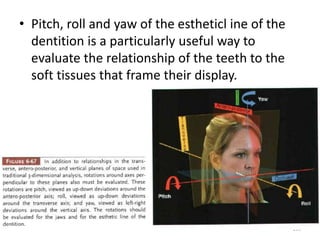
The document discusses orthodontic diagnosis, emphasizing the importance of various diagnostic aids, including patient history, clinical examination, and radiographs. It outlines a systematic approach for establishing a comprehensive diagnosis based on patient questioning, clinical evaluations, and diagnostic records. The text also details the implications of several medical conditions on orthodontic treatment and the impact of pharmacological agents on tooth movement.