- The document discusses cervical vertebral maturation (CVM) as a method to assess skeletal maturity based on morphological changes in cervical vertebrae visible on cephalometric radiographs.
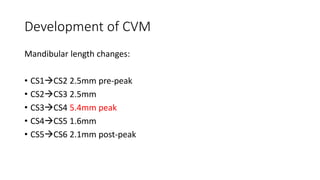
- CVM stages correlate well with peak periods of mandibular growth. Treatment is most effective targeting the growth spurt in CVM stages 3 and 4.
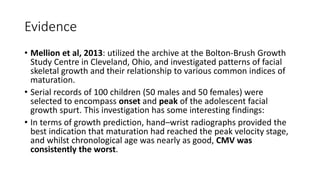
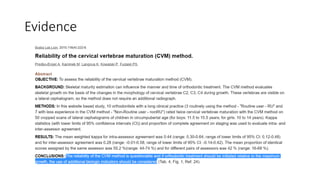
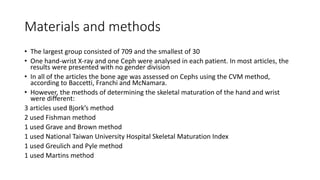
- A review of 10 studies found high correlations between CVM and hand-wrist maturation methods. While hand-wrist is the gold standard, the studies concluded CVM could replace it as an indicator of skeletal maturity.