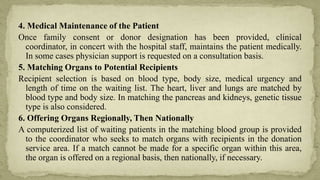
This document provides an overview of organ donation, including the definition of organ donation, types of organ donation (live vs. deceased donors), organs that can be donated, laws around organ donation, organizations involved in organ donation, and the process of organ donation and transplantation. Key points covered include that organs from a single donor can benefit many recipients, and that the first organ transplant was a kidney transplant in 1954 between identical twins.