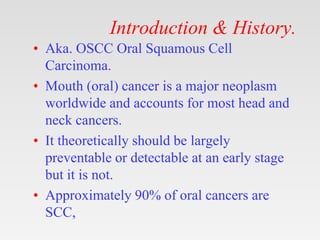
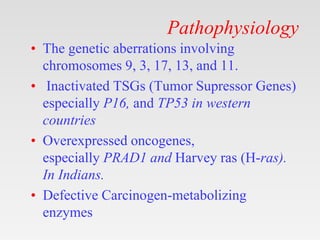
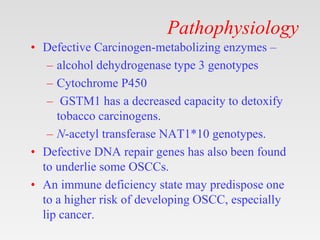
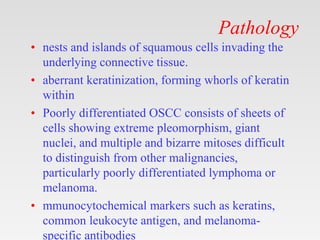
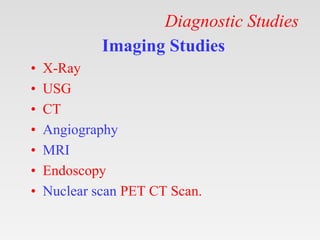
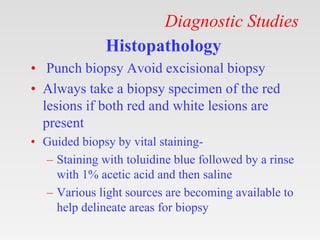
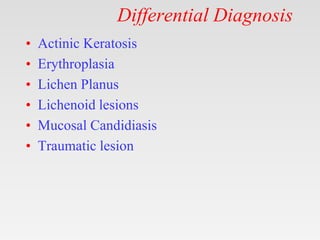
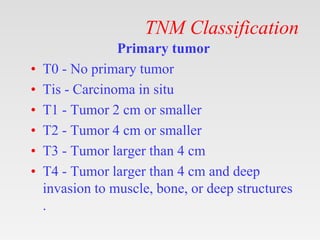
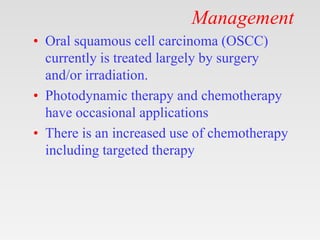
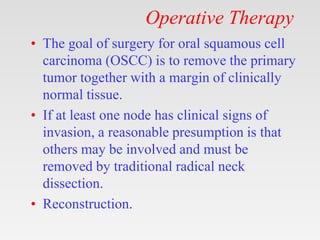
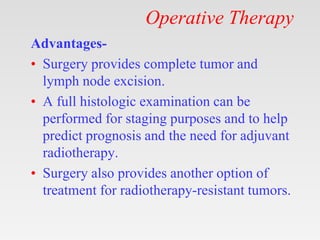
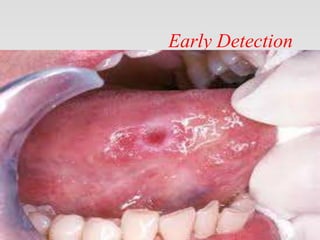
This document provides tips and instructions for using a PowerPoint presentation on oral squamous cell carcinoma (OSCC). It recommends showing blank slides with learning objectives and asking students what they know, then filling them in. This active learning technique should be repeated three times for revision. The presentation covers topics like etiology, pathology, clinical features, investigations and management of OSCC over 12 slides. It aims to be useful for both teaching and self-study.