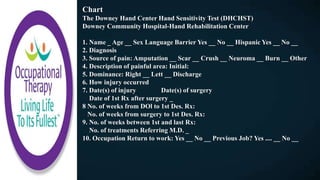
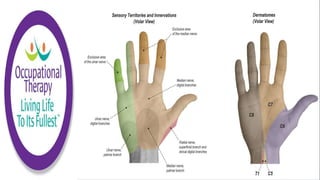
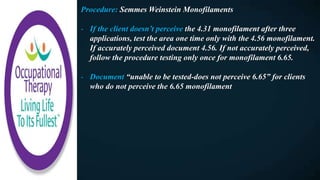
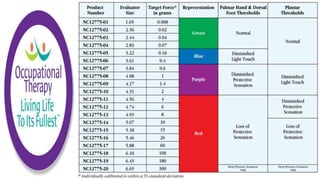
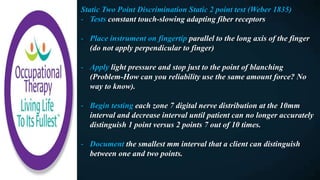
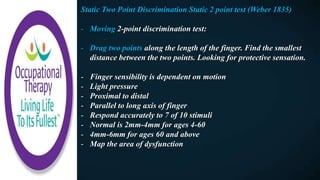
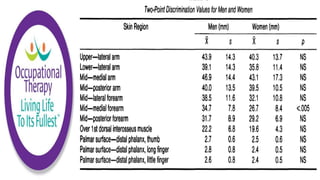
The document discusses various topics related to occupational therapy for sensory testing and assessment of the hands. It covers topics like protective sensation, hyperesthesia, pain assessment, and interventions like desensitization. Some key points include:
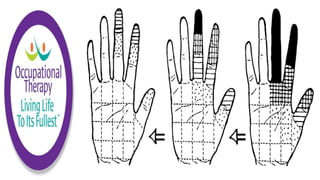
- Protective sensation allows the hands to sense pain and avoid injury, and patients who lose this need compensatory strategies. Hyperesthesia causes discomfort with touch and may be treated with desensitization.
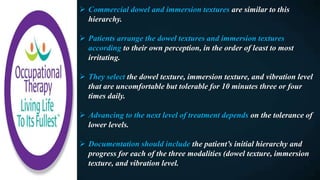
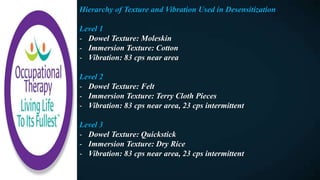
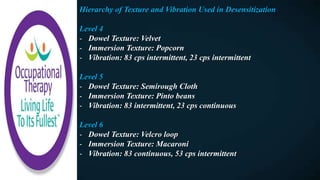
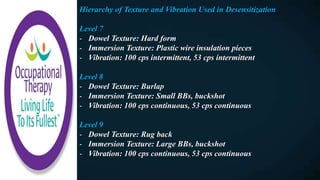
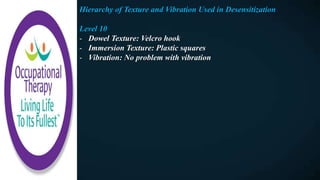
- Desensitization uses gradual exposure to textures of increasing intensity to increase tolerance to touch. Mirror therapy can help by giving the illusion of two normal limbs.
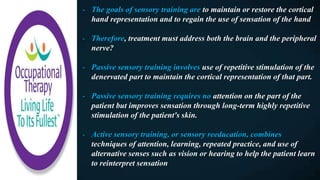
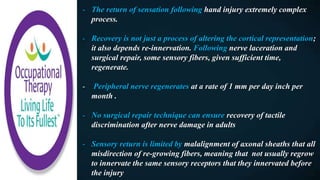
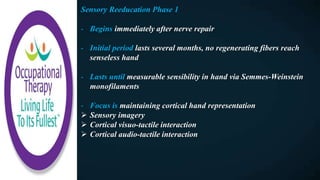
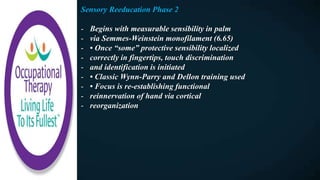
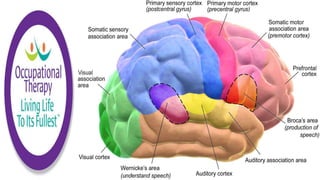
- Sensory training aims to maintain cortical representation of the hand and regain use of sensation. Passive training uses repetition while