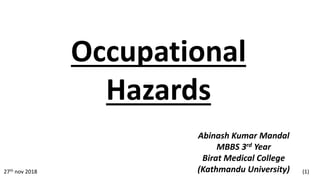
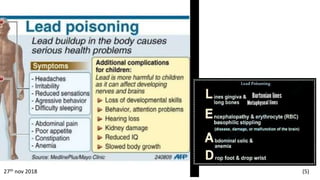
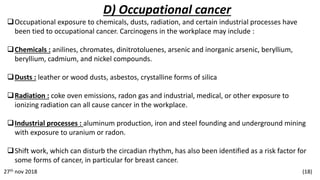
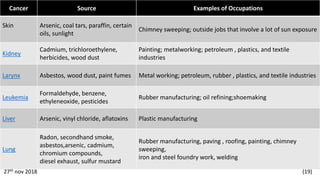
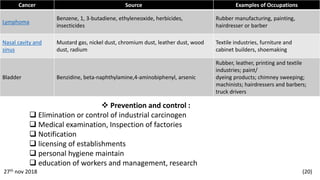
This document discusses various occupational hazards including lead poisoning from industries like smelting and recycling, radiation hazards from industries like nuclear power and medical imaging, occupational dermatitis from chemical exposure, occupational cancers caused by chemicals, dusts and radiation, and hazards for agricultural workers like zoonotic diseases, accidents, toxic chemicals and physical hazards. It provides details on the causes, health effects, treatments and preventive measures for many of these occupational hazards.