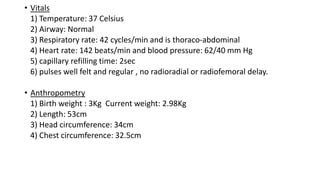
A 3 day old term male baby born via normal vaginal delivery is presented for routine newborn checkup. The baby was exclusively breastfed with normal growth parameters. Physical examination revealed a well-developed baby with normal vital signs and systemic examination. The baby is being provided with normal newborn care.