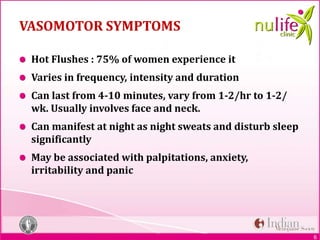
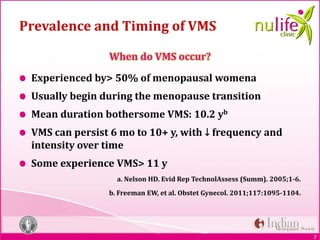
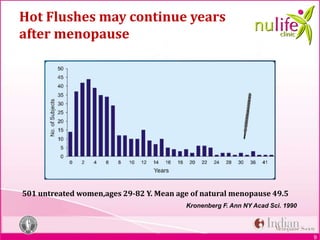
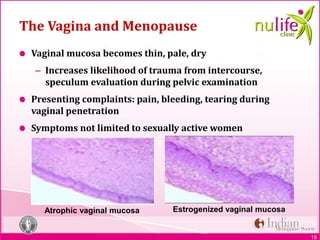
The document discusses symptoms of menopause. It describes common vasomotor symptoms like hot flashes that affect over 50% of menopausal women, as well as psychological, sleep, genitourinary, and sexual symptoms. It provides details on evaluating a patient in menopause through history, physical exam, and screening for risks. It also presents a case study of a patient experiencing hot flashes and discusses appropriate counseling and management.