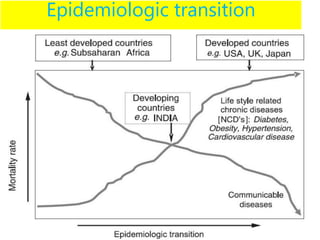
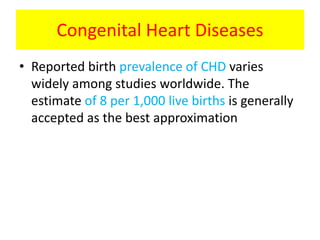
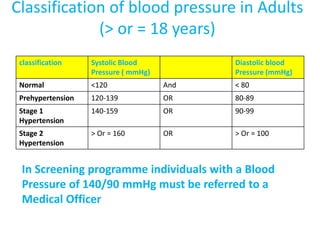
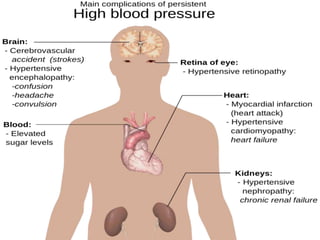
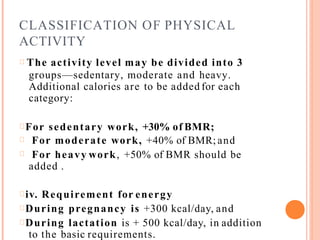
The document discusses the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) in India. It summarizes that NPCDCS aims to prevent and control four major non-communicable diseases through strengthening infrastructure, human resource development, health promotion, early diagnosis, and management/referral. It also briefly outlines the burden and risk factors of cardiovascular diseases, highlighting they are a leading cause of death in India and globally.