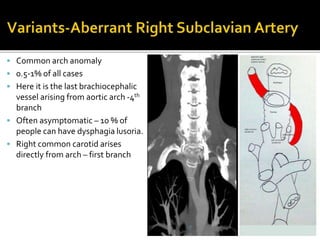
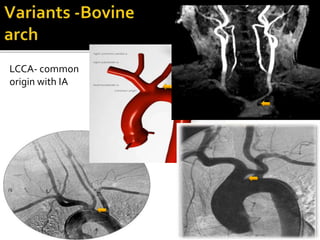
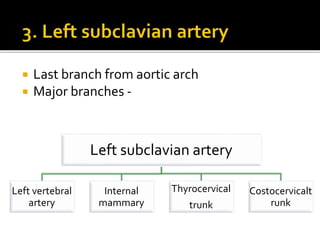
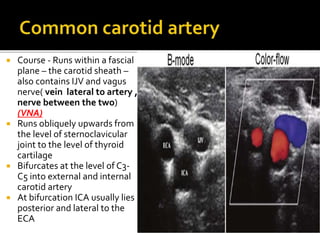
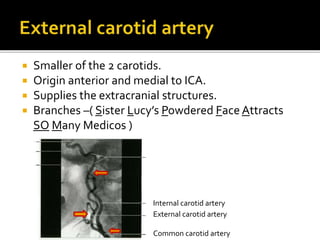
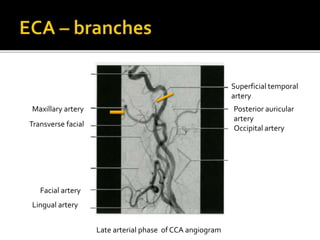
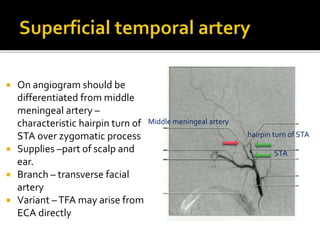
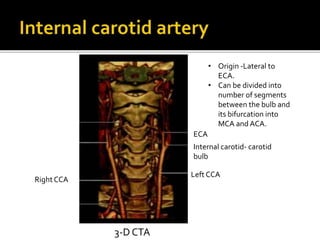
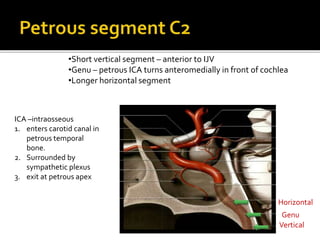
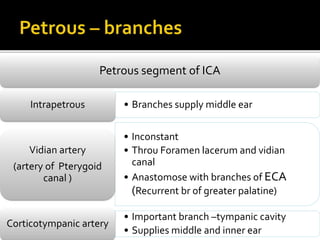
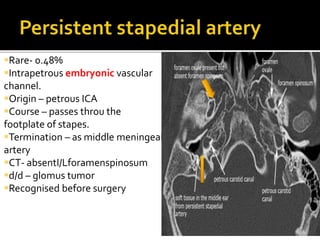
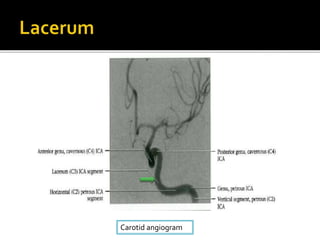
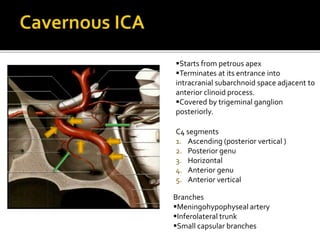
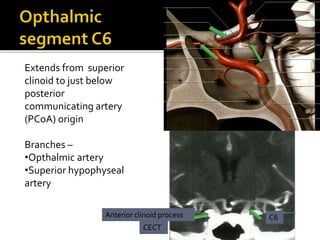
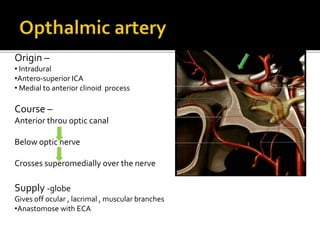
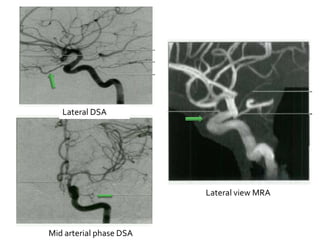
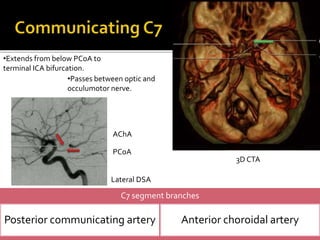
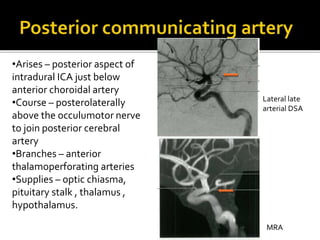
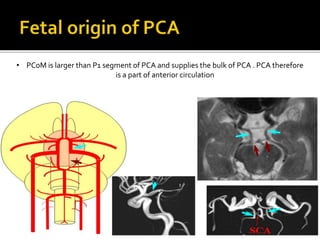
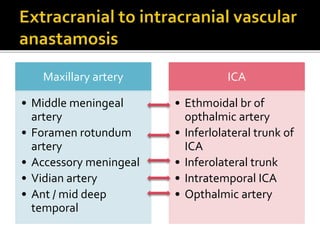
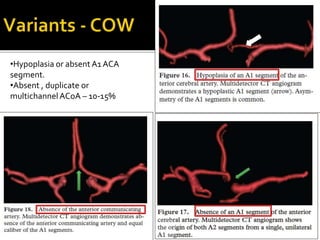
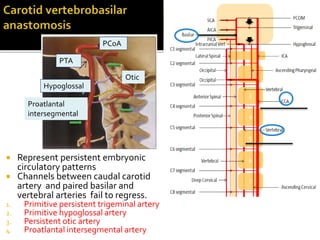
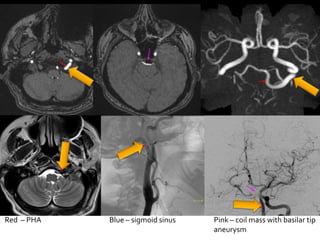
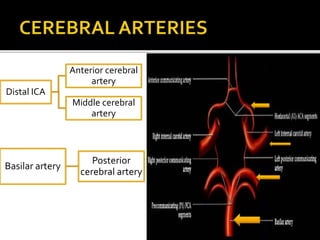
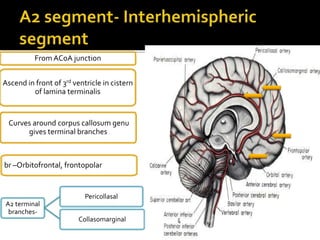
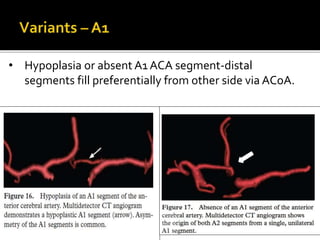
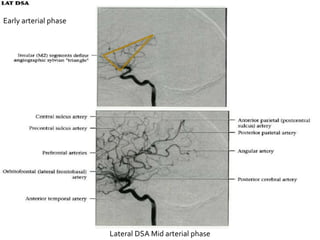
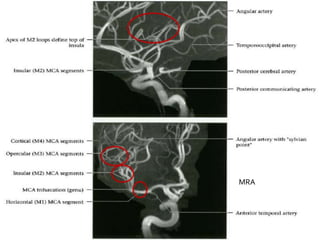
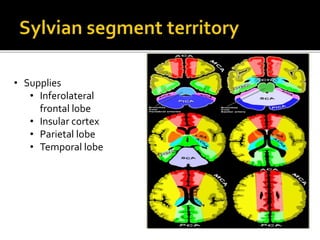
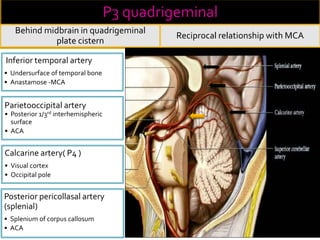
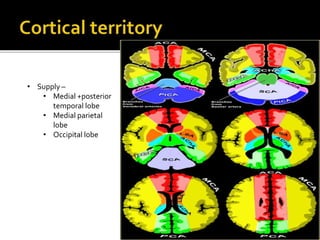
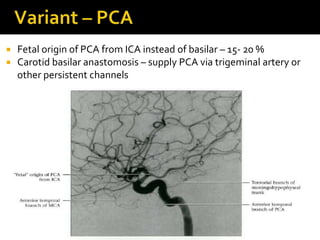
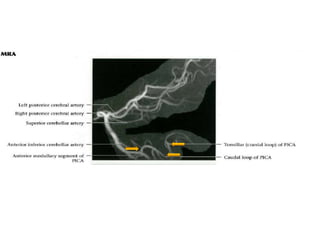
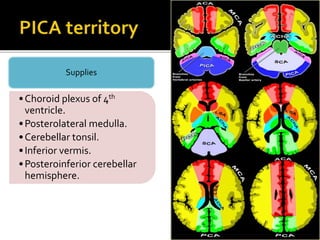
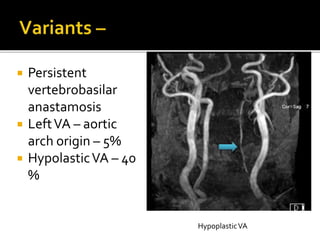
The document discusses vascular anatomy of the brain. It notes that 18% of total blood volume circulates through the brain, which accounts for 2% of body weight. Loss of consciousness occurs within 15 seconds and irreversible brain damage within 5 minutes if blood flow to the brain stops. It then describes the various arteries that supply the brain, including the carotid arteries, vertebral arteries, and branches within the brain. It provides details on imaging techniques used to evaluate the vasculature such as angiography, CTA, MRA. Overall, the document provides an overview of the anatomy and imaging of brain vasculature.