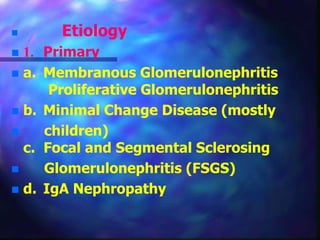
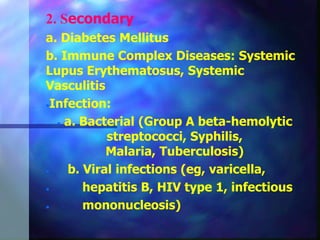
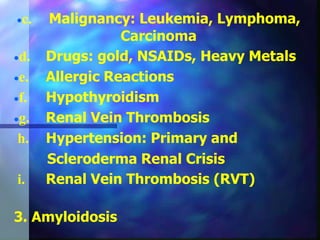
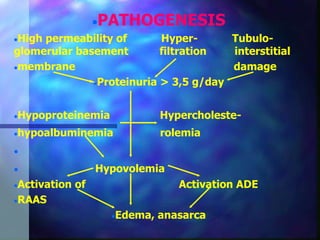
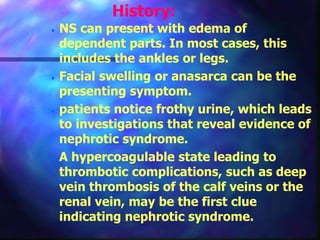
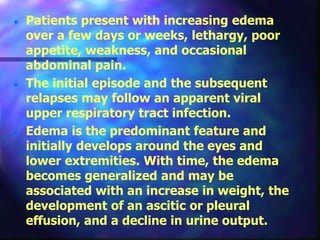
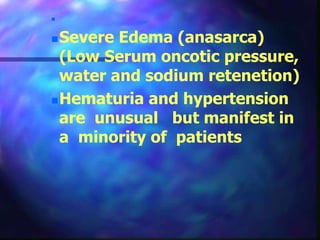
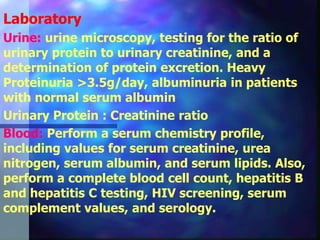
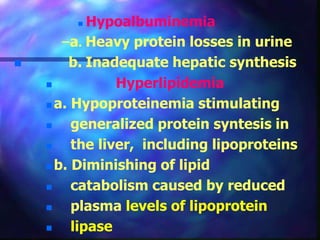
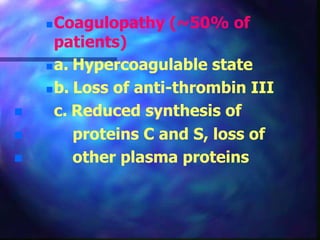
Nephrotic syndrome is characterized by heavy proteinuria, hypoalbuminemia, edema, and normal kidney function. It has multiple primary and secondary causes, including diseases like membranous glomerulonephritis or diabetes. Patients present with edema, fatigue, and abdominal pain. Laboratory tests show protein in the urine and low serum albumin. Treatment involves addressing the underlying cause, diuretics, and immunosuppressants like prednisone. Complications can include infections, blood clots, and kidney damage if left untreated.