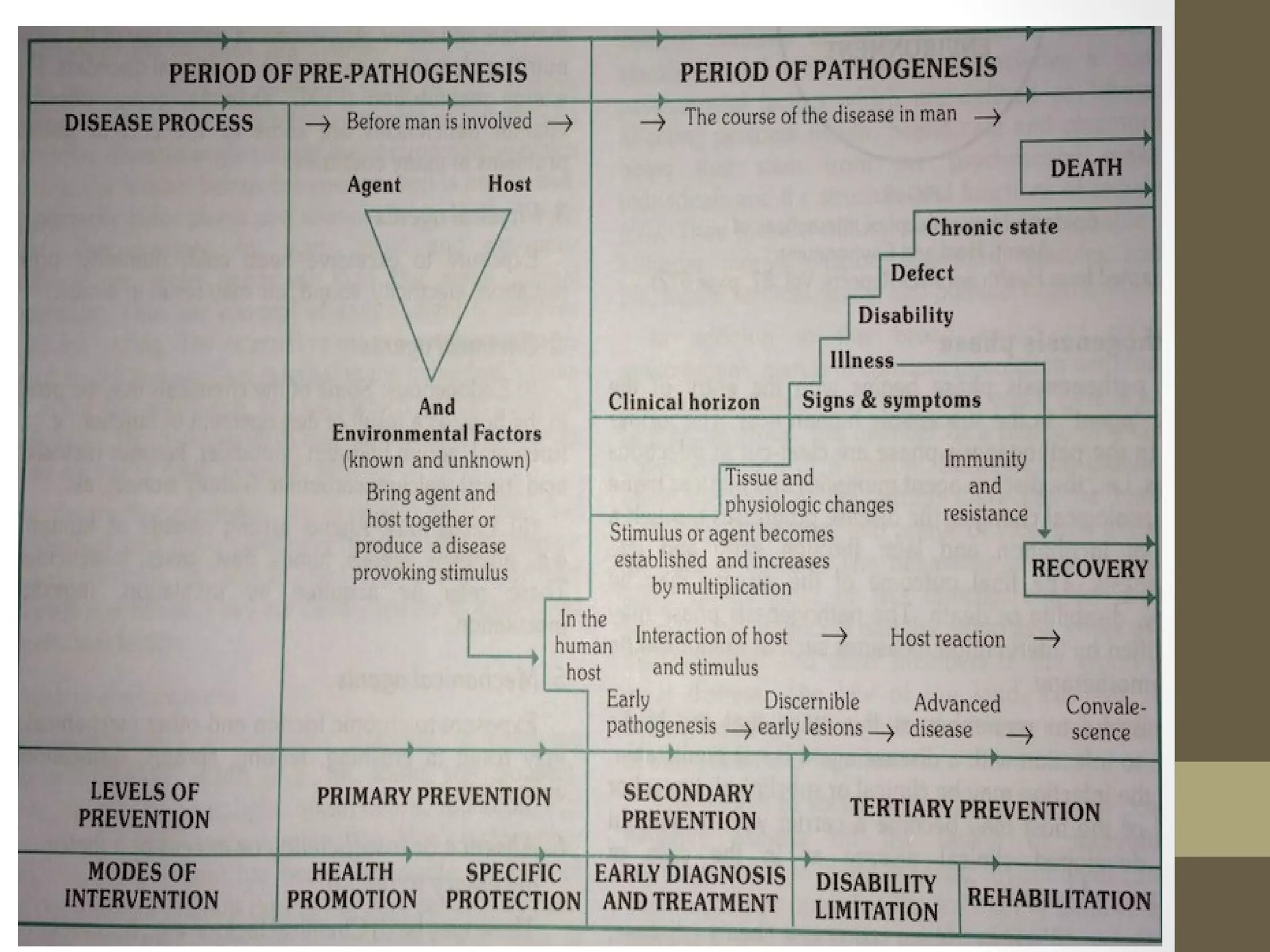
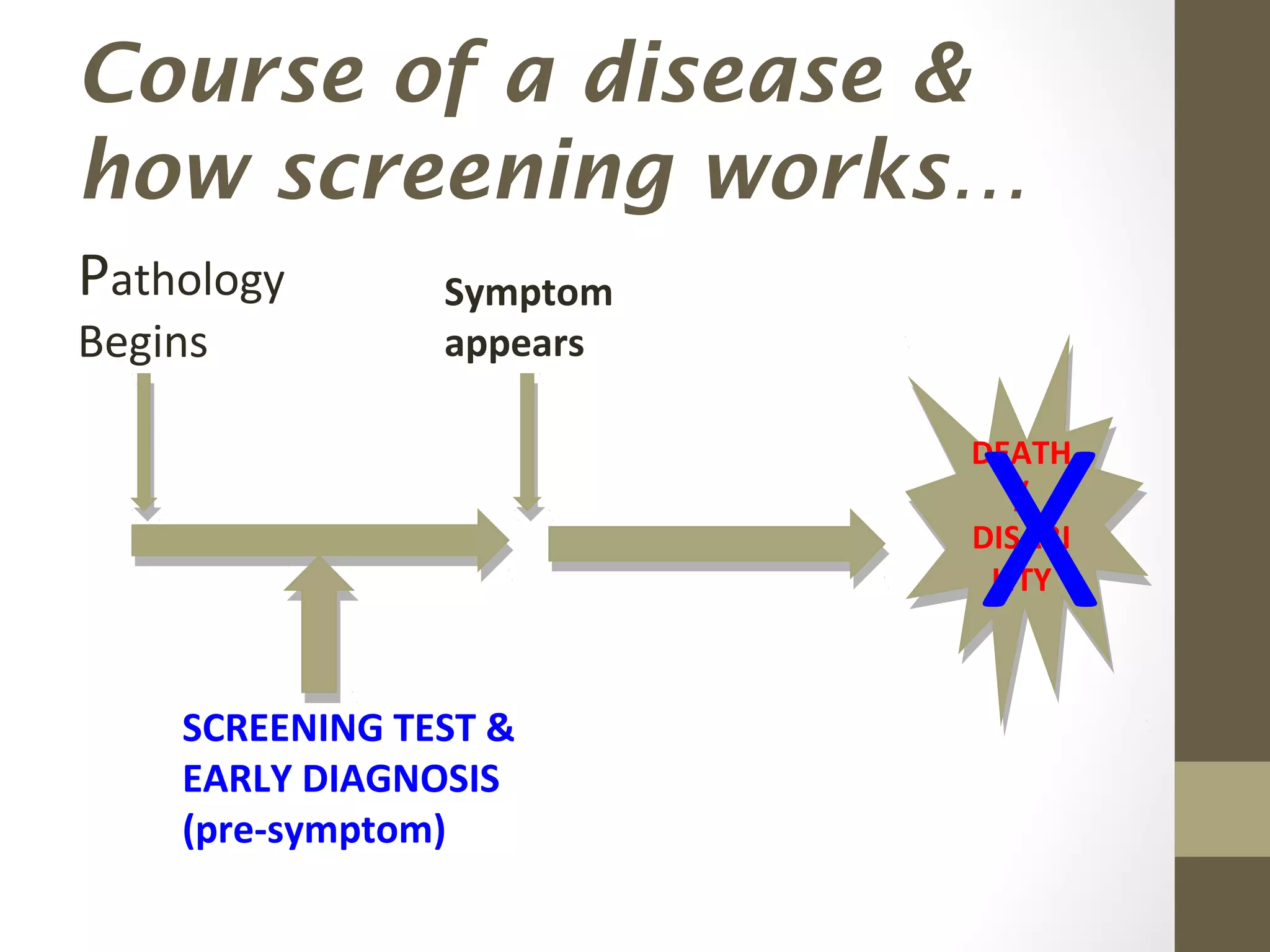
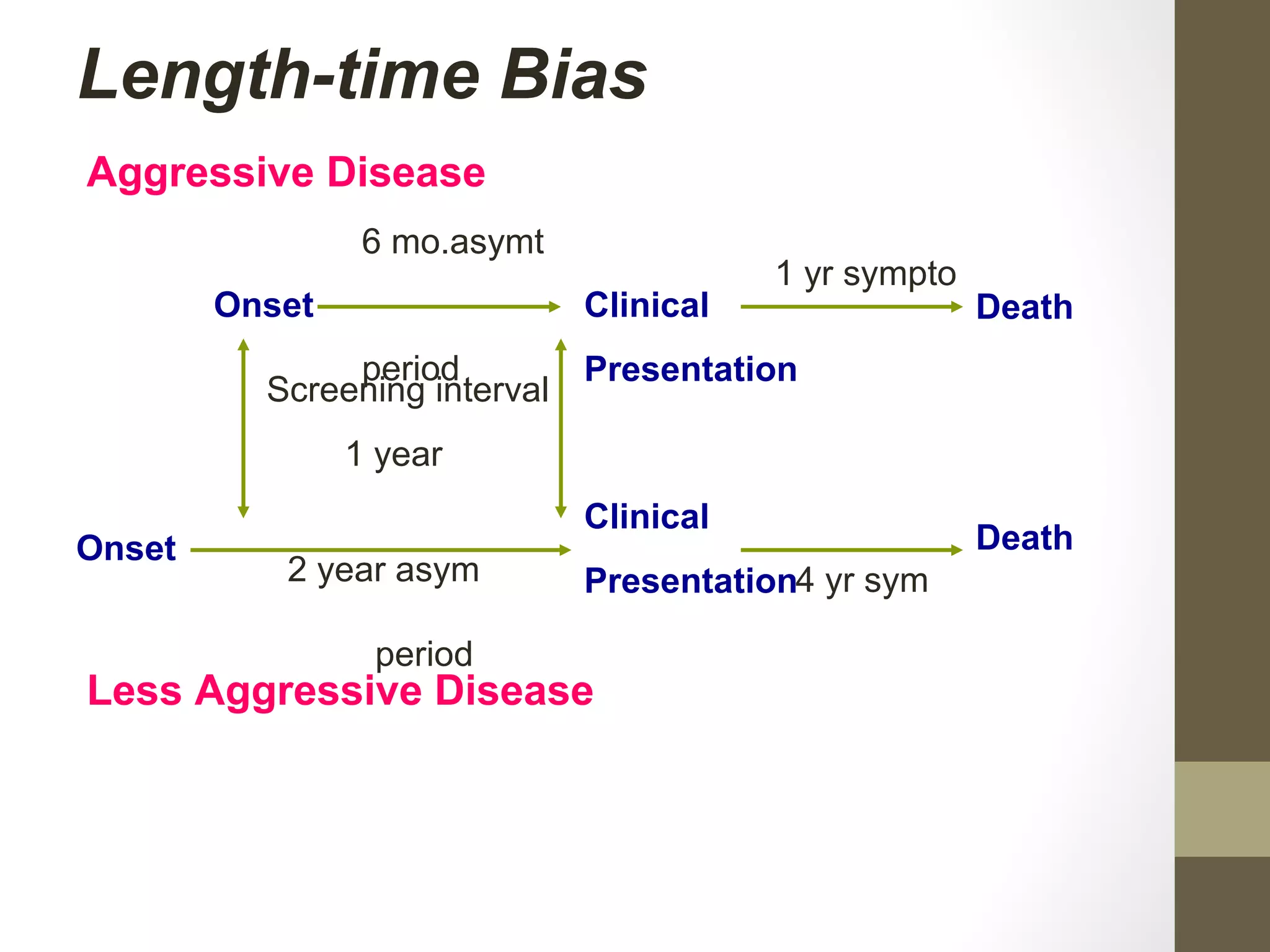
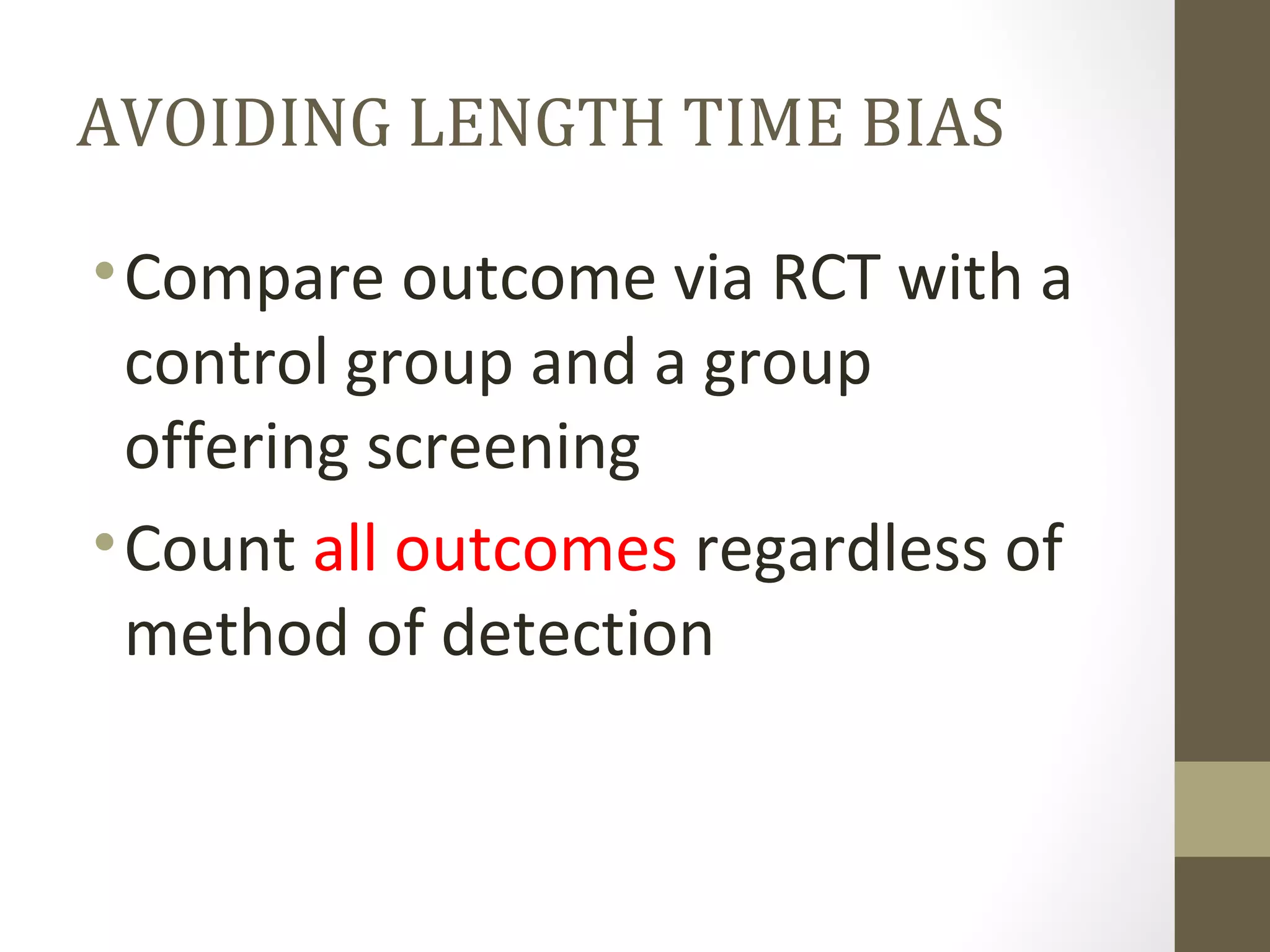
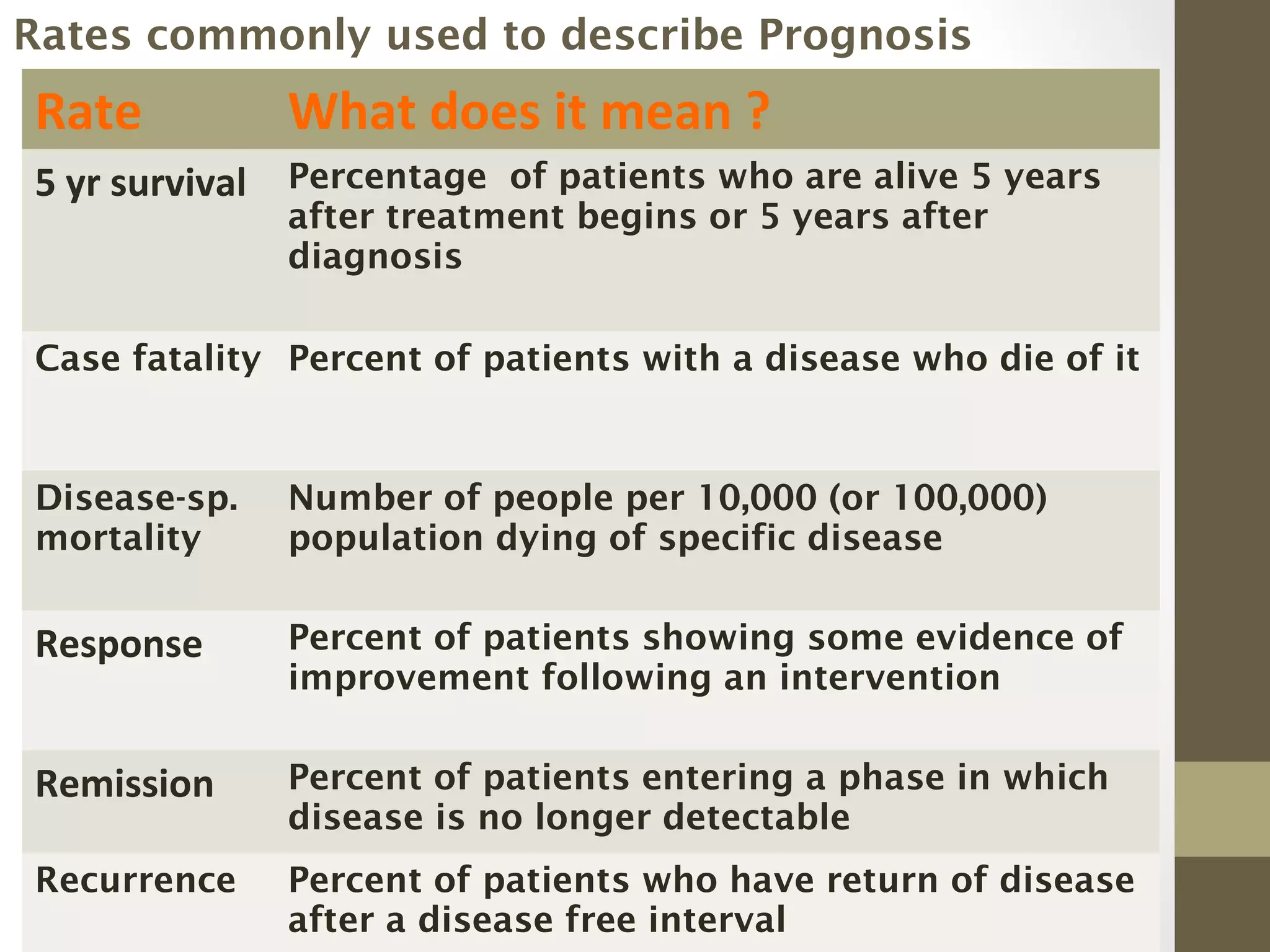
The document discusses the natural history of diseases, defining stages from pre-pathogenesis to pathogenesis, and emphasizes the importance of understanding these stages for effective disease prevention and screening. It outlines three levels of prevention: primary, secondary, and tertiary, detailing respective strategies for intervention at different disease stages. Additionally, it addresses concepts like lead time bias and length time bias in screening, and the necessity of prognostic evaluations in assessing disease treatment outcomes.