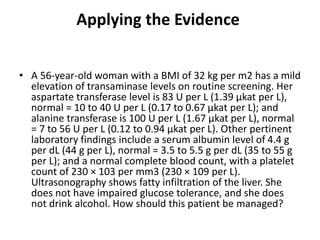
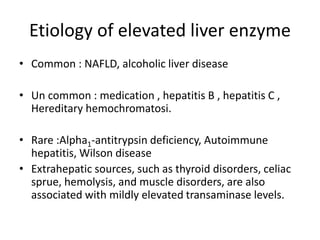
This document discusses two cases of patients with elevated liver enzymes. For the first case, a 35-year old man tests positive for hepatitis B surface antigen, indicating chronic hepatitis B infection. The document outlines the appropriate history, physical exam, laboratory tests, and imaging needed to evaluate elevated liver enzymes. For the second case, a 38-year old woman was found to have fatty liver on ultrasound. The document then summarizes nonalcoholic fatty liver disease including causes, risk factors, evaluation, and treatment recommendations.




![History
• often asymptomatic, but symptoms may include right
upper quadrant pain, jaundice, and pruritus.
• R/o possible causes for liver dx : alcohol and drug use, risk
factors for viral hepatitis, including intravenous drug use,
blood transfusion, and sexual activities.
- The history should explore diet, physical activity, change in
weight (usually an increase, such as 40 lb [18 kg] over two
to three years),
- Associated conditions (e.g., diabetes, hypertension,
hyperlipidemia, obesity, sleep apnea).
- The patient's family history should be checked for
cardiovascular and metabolic disorders, and chronic liver
disease](https://image.slidesharecdn.com/nafldraisedlft-180305082312/85/Nafld-raised-lft-5-320.jpg)











![Risk factor
• age older than 45 years,
• an alanine transaminase (ALT) level greater than
the an aspartate transaminase (AST) level
• diabetes, insulin resistance
• low albumin level (less than 3.6 g per dL [36 g per
L])
• low platelet count (less than 100 × 103 per μL
[100 × 109 per L])
• metabolic syndrome, obesity
• portal hypertension on imaging](https://image.slidesharecdn.com/nafldraisedlft-180305082312/85/Nafld-raised-lft-19-320.jpg)

![NONINVASIVE TESTS FOR LIVER
FIBROSIS
the aspartate transferase to platelet ratio index
the alanine transferase ratio
the BARD score, 5 which comprises the weighted sum of
three variables (body mass index [BMI] of 28 kg per m2 or
more, aspartate transferase to alanine transferase ratio,
and the presence of diabetes mellitus).
The FIB-4 score has similar variables as the aspartate
transferase to platelet ratio index, with the addition of age.
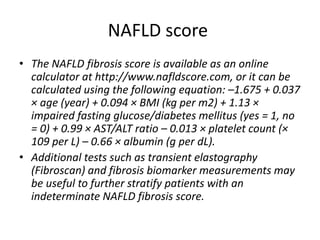
the NAFLD fibrosis score includes age, BMI, blood glucose
levels, transferase levels, platelet count, and albumin levels
magnetic resonance elastography](https://image.slidesharecdn.com/nafldraisedlft-180305082312/85/Nafld-raised-lft-21-320.jpg)