**Activity and Exercise Nursing** refers to the role of nurses in promoting, planning, and assisting with physical activity and exercise as part of patient care. This approach aims to improve or maintain a patient's physical health, mobility, and overall well-being. Nurses assess a patient’s physical condition, provide guidance on safe exercise practices, and monitor progress throughout the process.
### Key Components of Activity and Exercise Nursing:
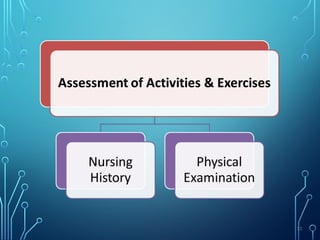
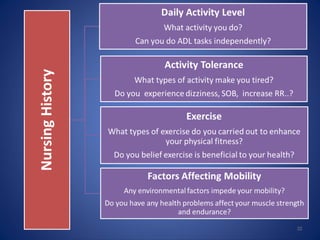
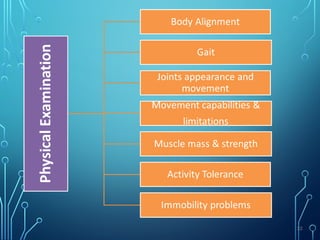
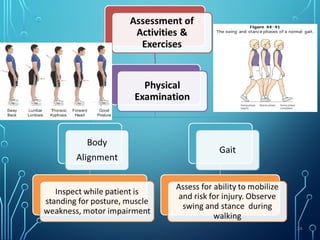
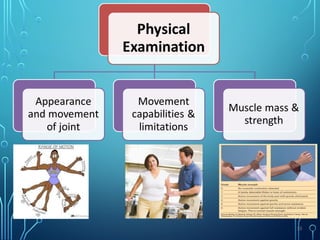
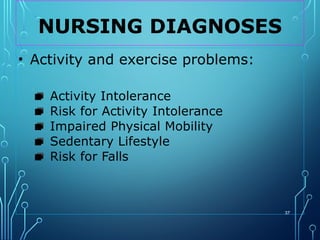
1. **Assessment of Physical Function:**
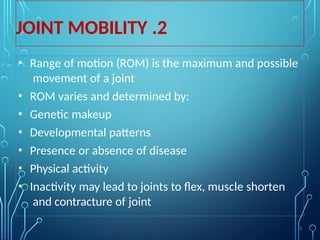
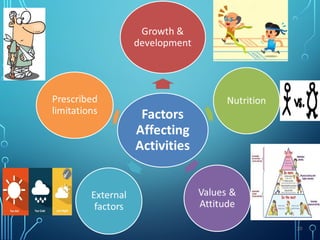
Nurses assess a patient's baseline activity level, range of motion, and overall physical health to determine appropriate activity goals. This includes considering factors such as age, chronic conditions (e.g., cardiovascular disease, diabetes), and current functional status.
2. **Exercise Prescription:**
Nurses often collaborate with other healthcare providers, such as physical therapists, to create individualized exercise plans that meet the patient’s specific needs. This could involve aerobic exercise, strengthening exercises, or flexibility training, depending on the patient’s health condition.
3. **Patient Education:**
Nurses educate patients about the importance of physical activity in managing their condition or promoting recovery. This includes teaching patients how to perform exercises correctly, how often to do them, and any modifications needed based on their health status.
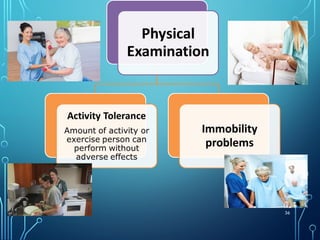
4. **Monitoring and Support:**
Nurses monitor the patient’s response to physical activity, including vital signs, signs of fatigue, pain, or discomfort. They provide encouragement and motivation while ensuring that exercise is safe and effective.
5. **Encouragement of Independence:**
In some cases, nurses aim to encourage patients to become more independent in their exercise routines, especially for those with chronic conditions or recovering from surgery. Nurses may suggest home-based exercises or guide patients to exercise programs that they can follow on their own.
6. **Collaborative Care:**
Nurses often work with physiotherapists, occupational therapists, and other healthcare professionals to ensure that exercise interventions align with the patient's overall treatment plan and health goals.
### Benefits of Activity and Exercise Nursing:
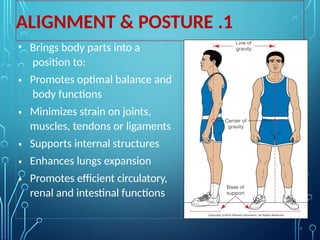
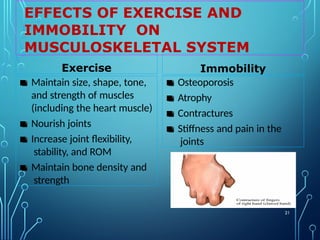
- **Improved Mobility**: Helps patients regain strength and independence.
- **Enhanced Circulation**: Boosts blood flow and reduces the risk of cardiovascular problems.
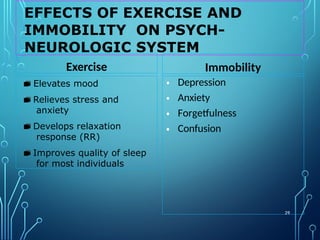
- **Better Mental Health**: Regular exercise has proven benefits for mental well-being, reducing stress, anxiety, and depression.
- **Prevention of Complications**: Regular physical activity helps prevent complications from conditions like diabetes, obesity, and heart disease.
Overall, activity and exercise nursing is a vital aspect of holistic patient care, ensuring that patients are encouraged and supported in maintaining or improving their physical health through safe and effective physical activity.