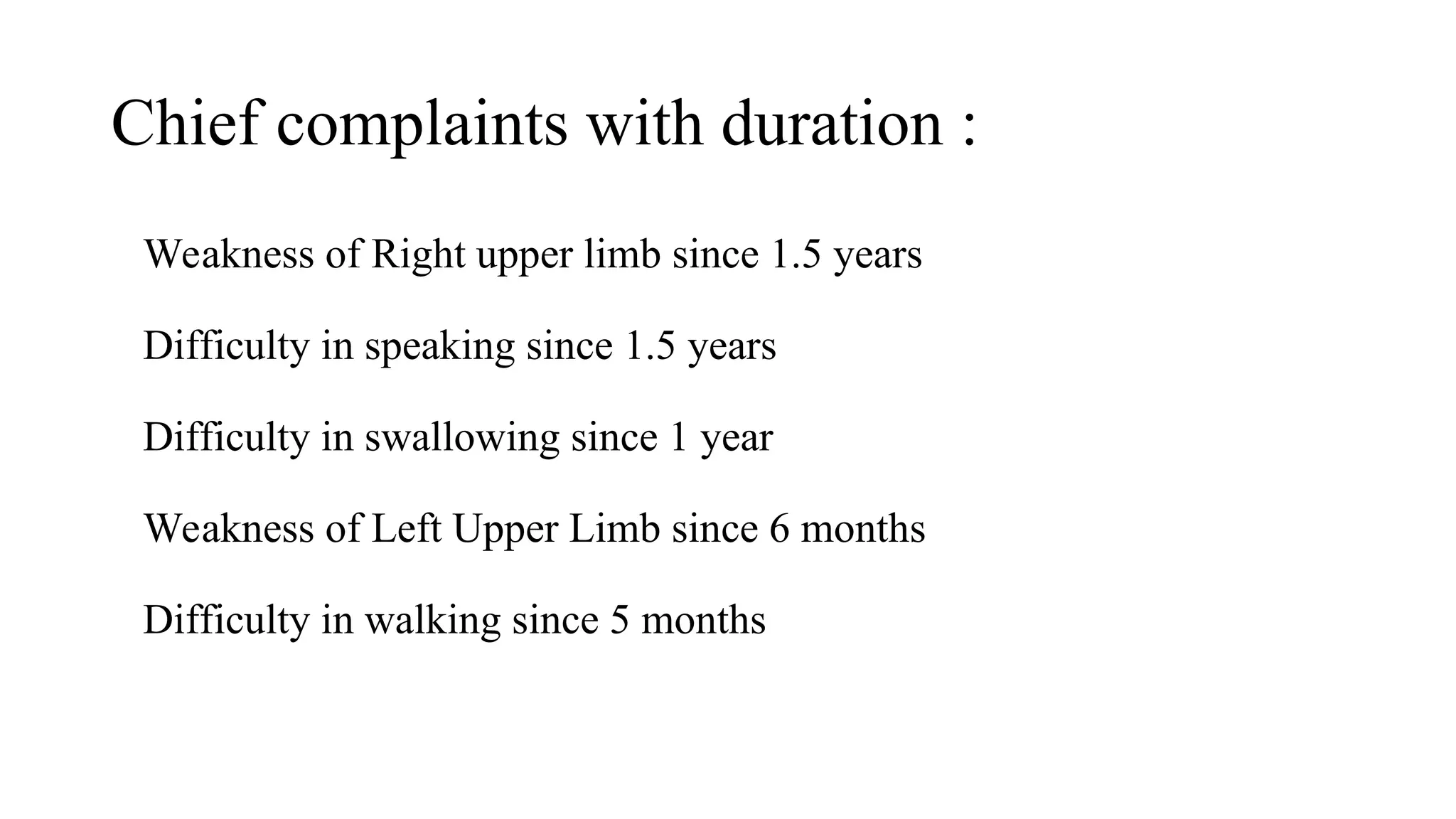
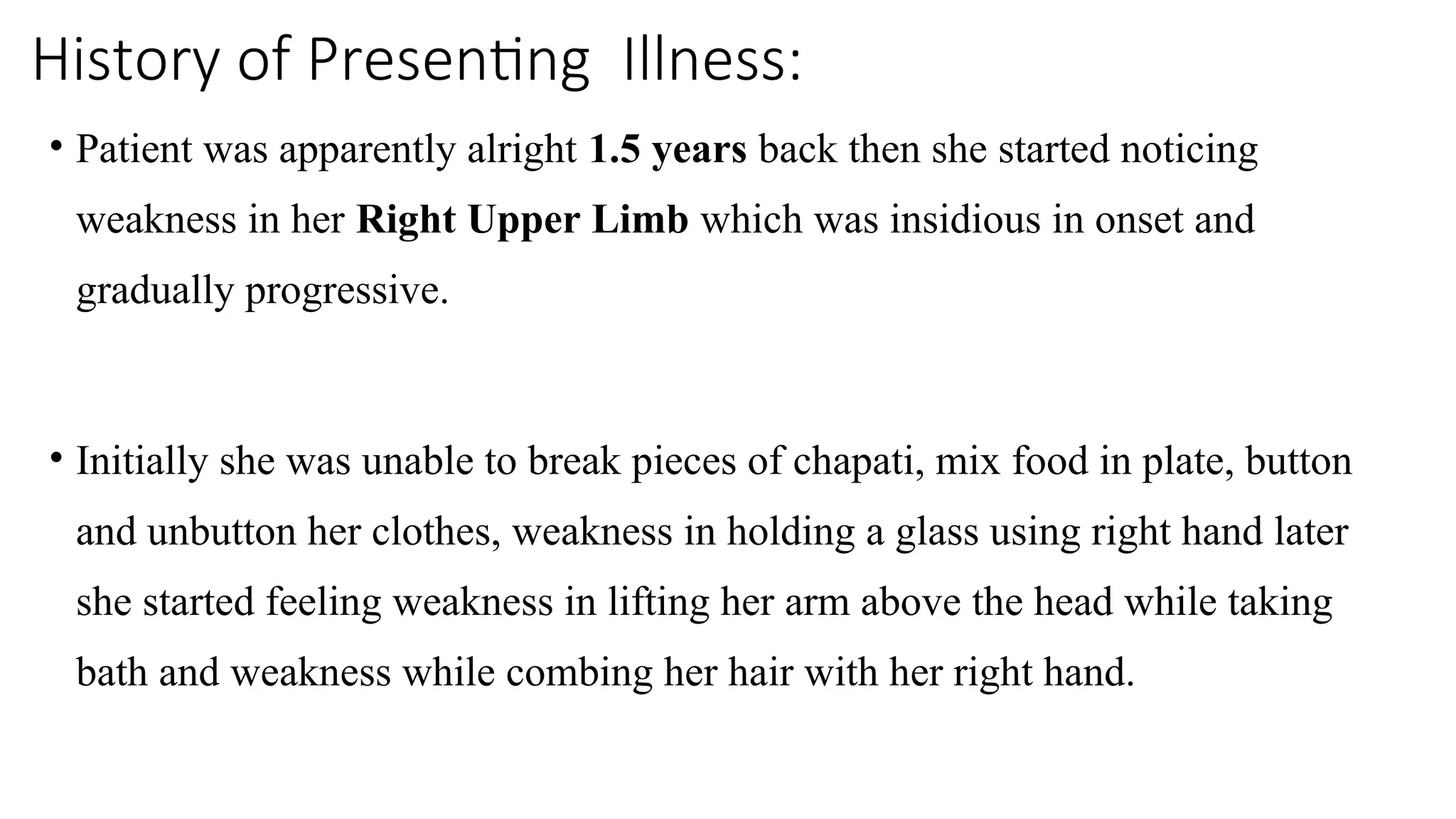
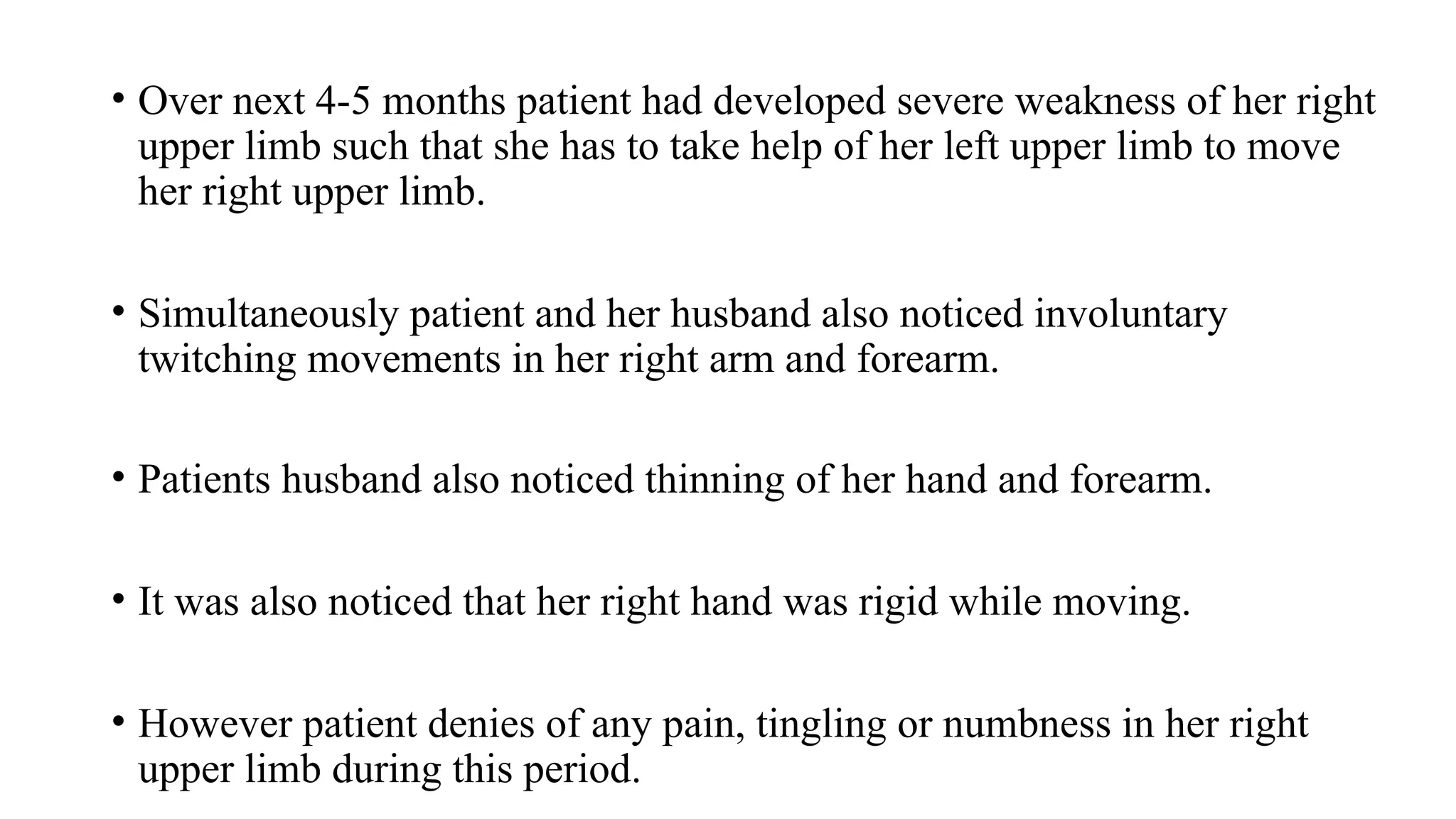
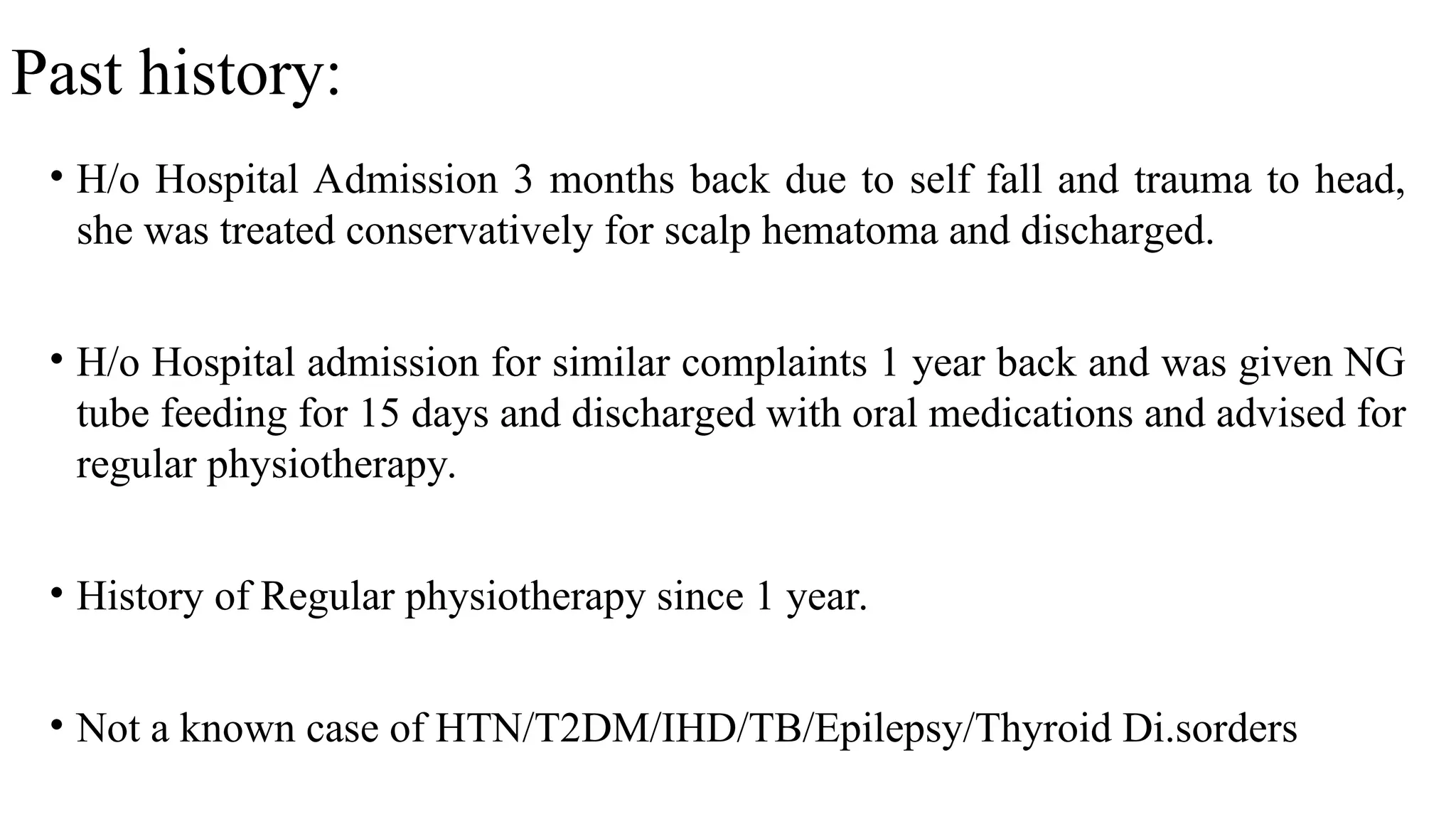
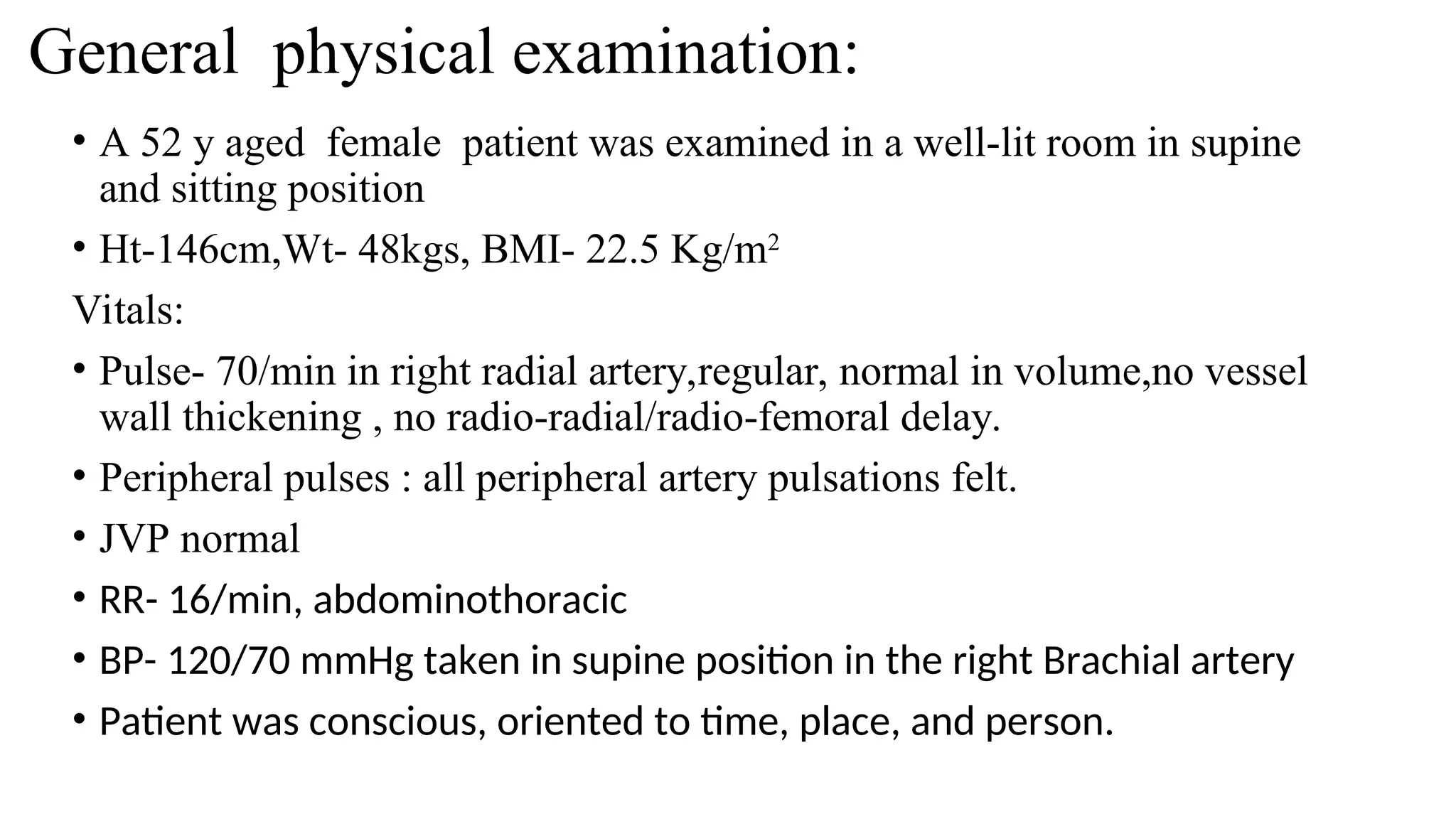
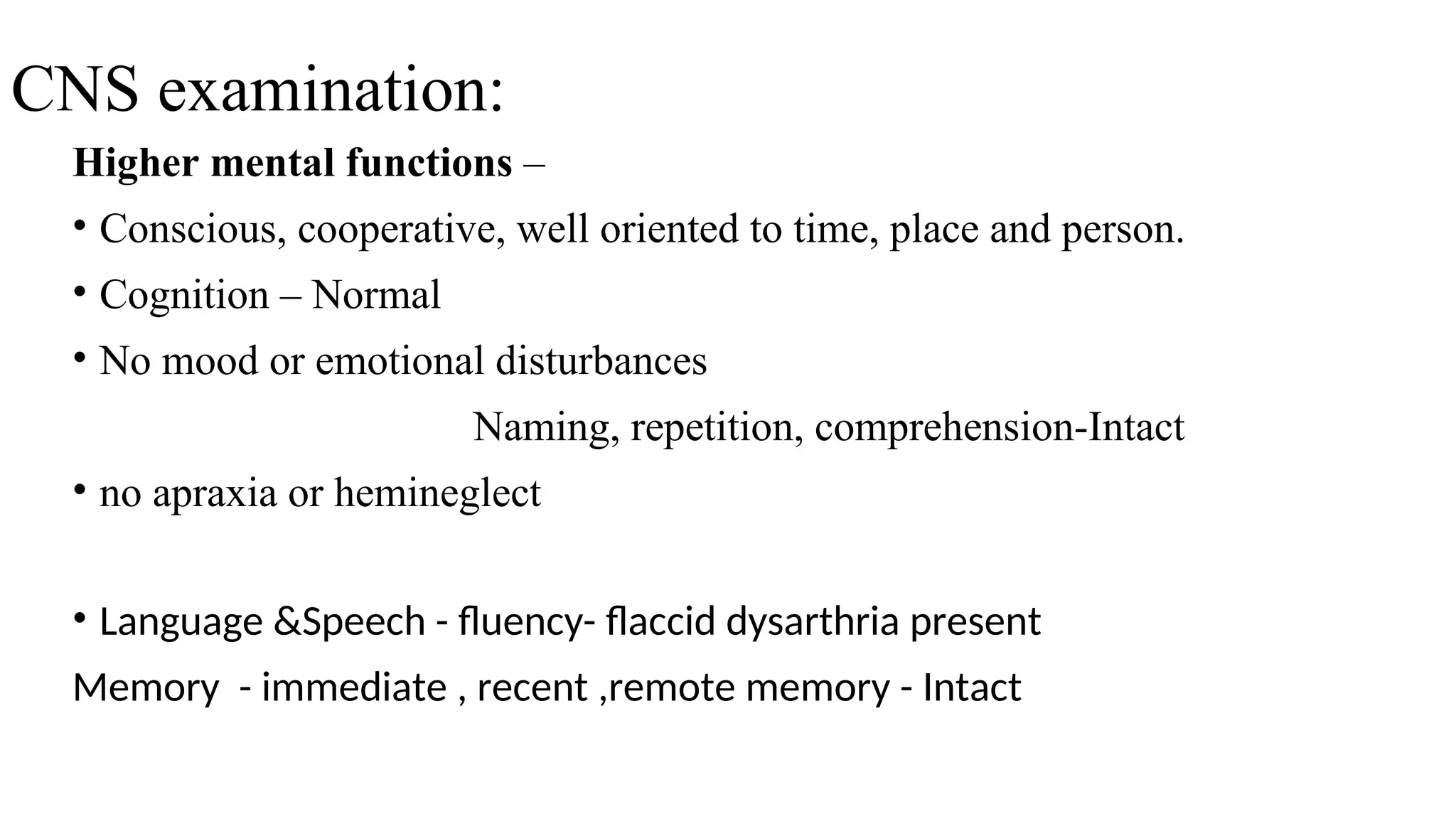
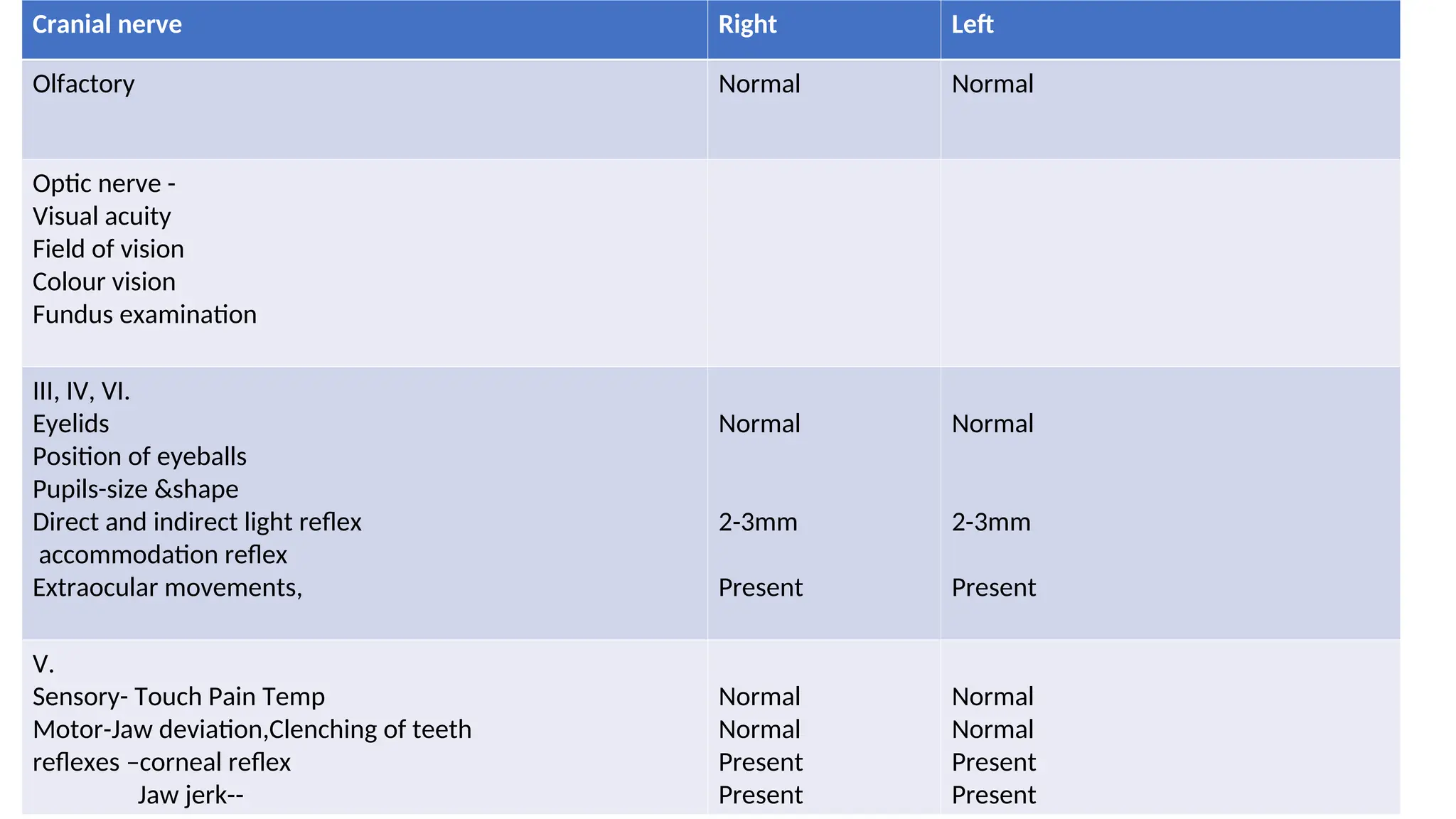
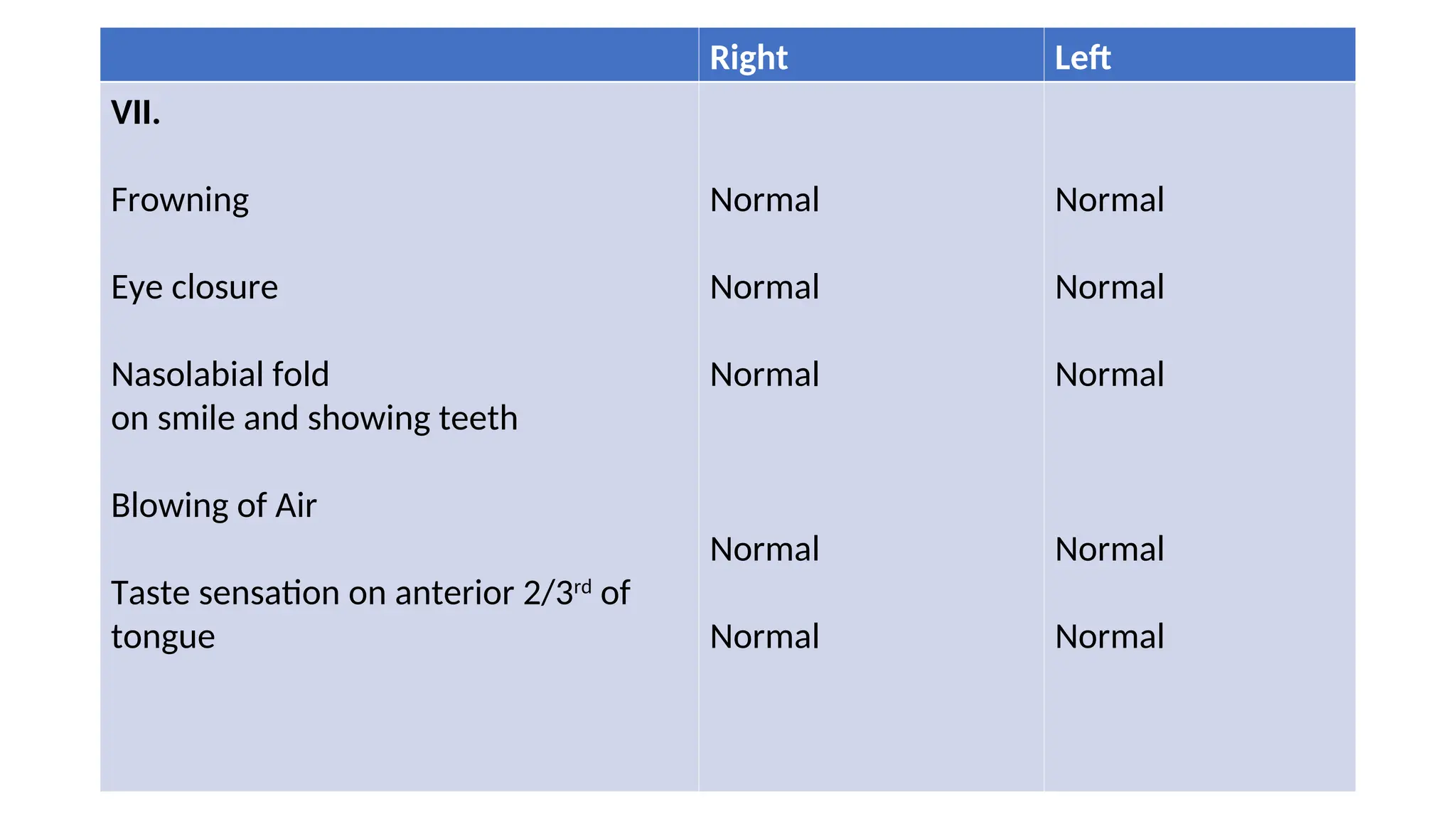
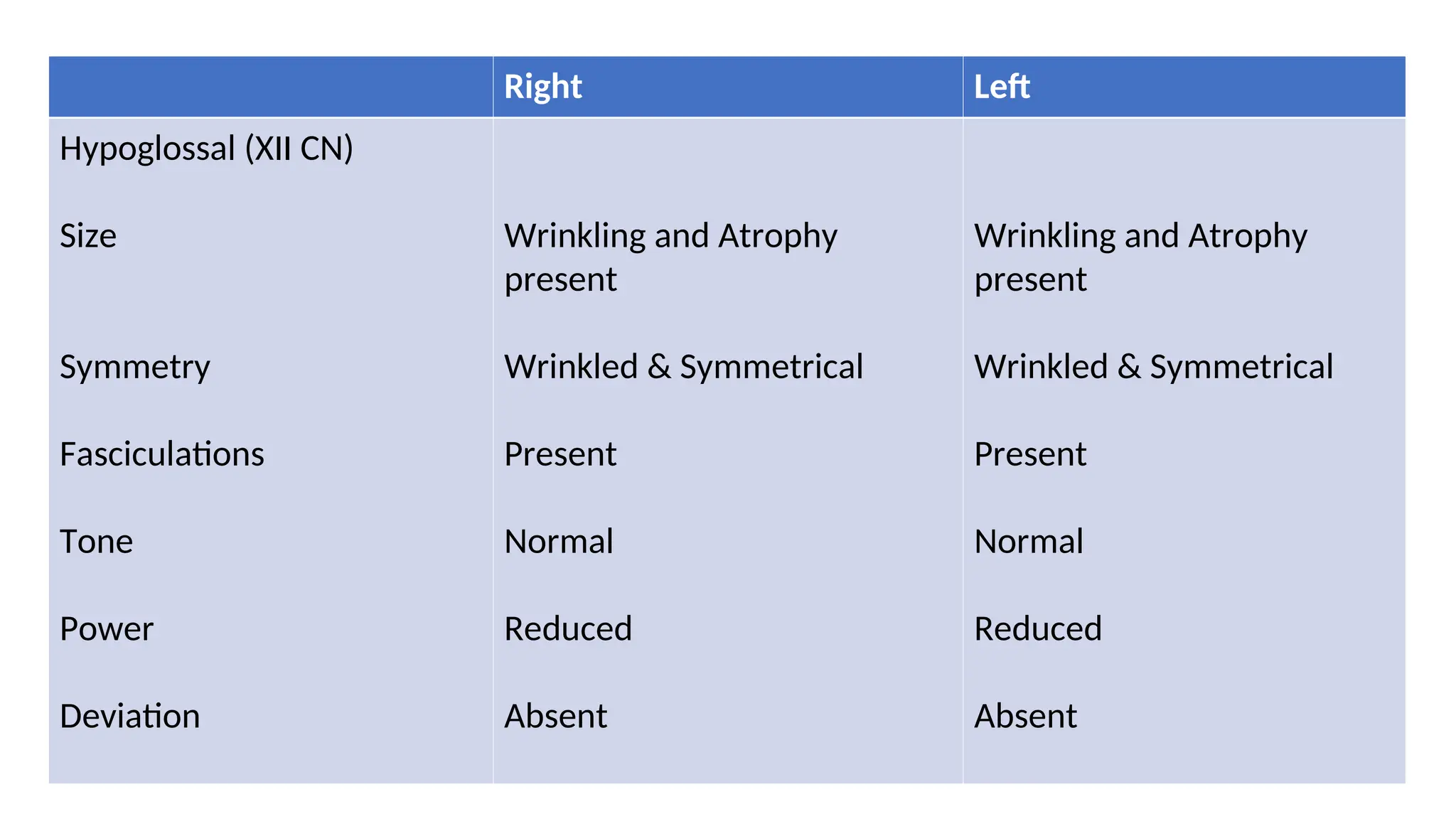
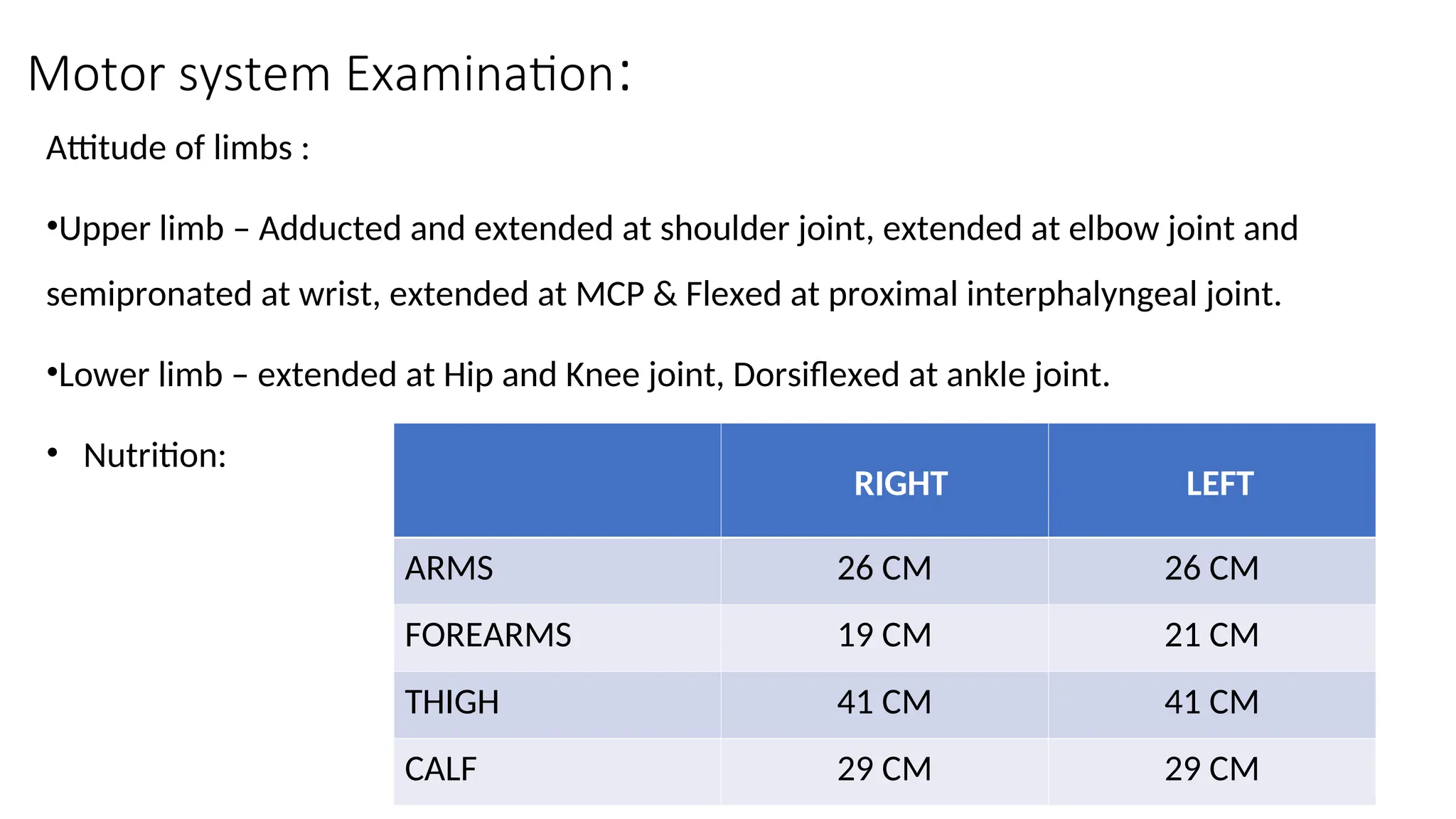
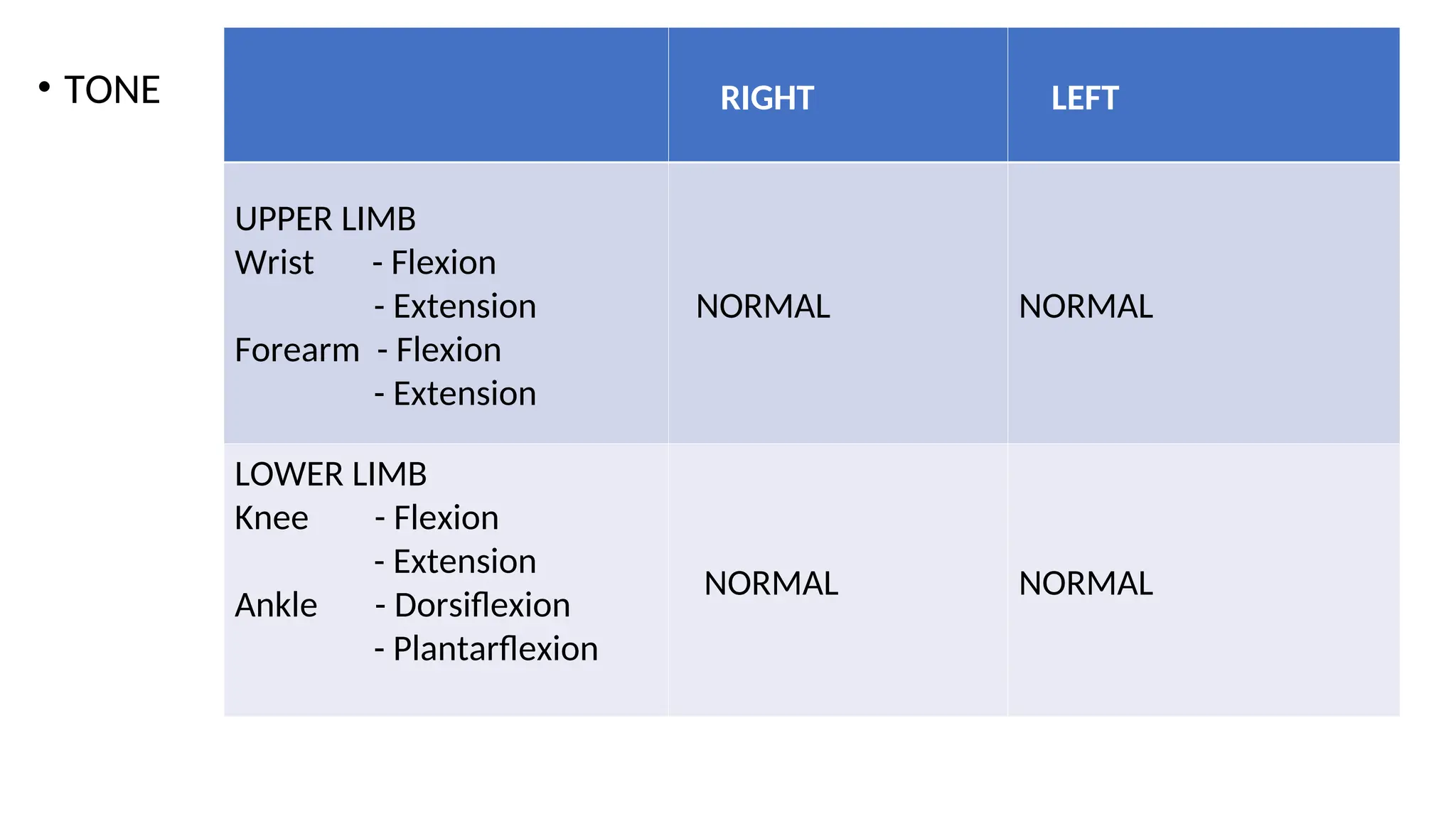
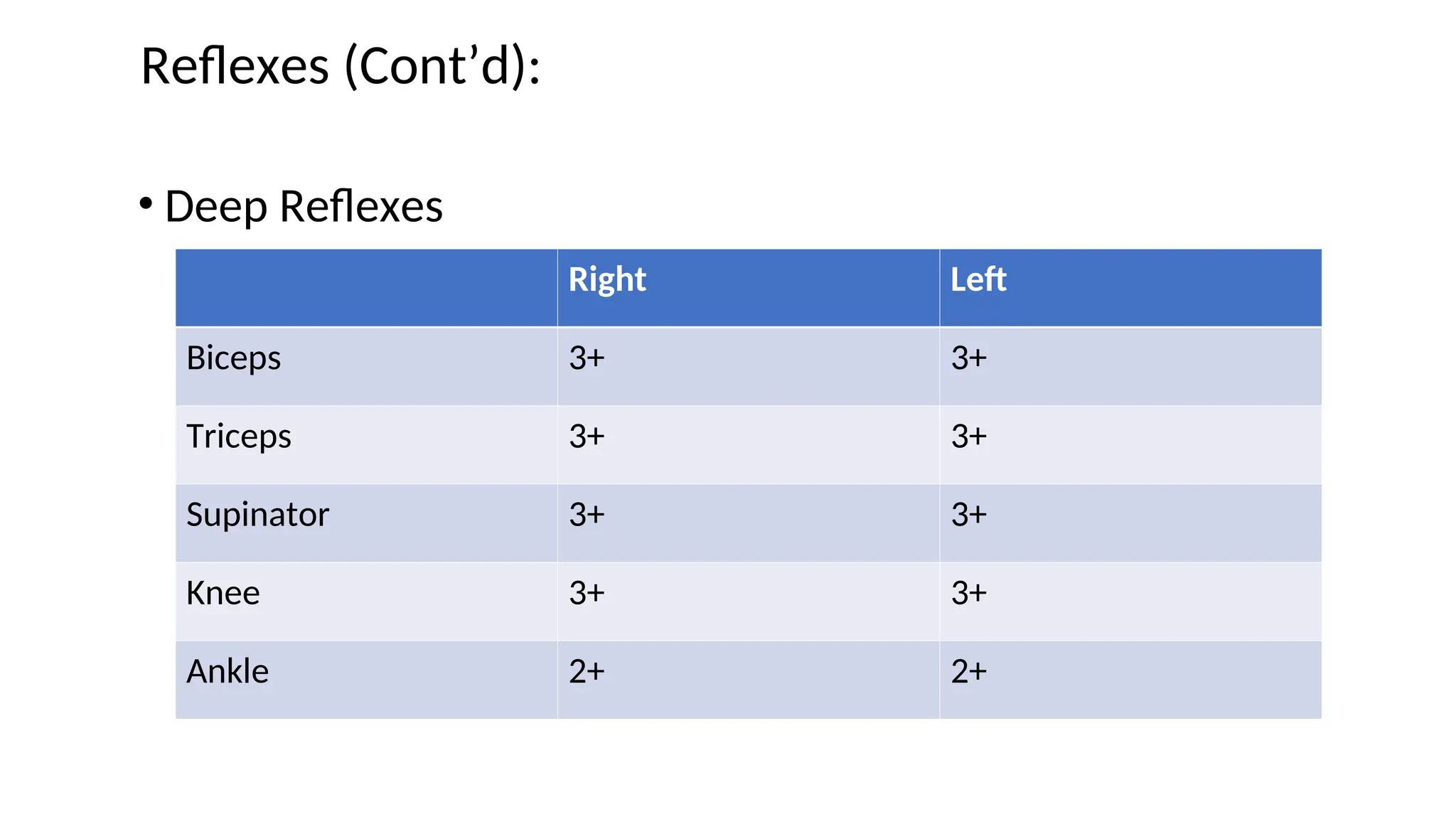
The document presents a case study of a 52-year-old female patient experiencing progressive weakness in her limbs, speech difficulties, and swallowing issues over 1.5 years. The examination reveals significant motor weakness and signs of bulbar palsy without sensory symptoms or cognitive impairments, and her history includes previous hospital admissions for similar complaints. The diagnosis suggests possible central nervous system involvement with a degenerative etiology.