This document provides information about microbiology for a B.Sc nursing course. It includes definitions of key terms like medical microbiology and Koch's phenomenon. It discusses the contributions of Robert Koch and Joseph Lister to the field. The document is divided into units, with the first unit covering an introduction and the second covering general characteristics of microbes. It includes short answer and essay questions about topics like bacterial cell structures, staining techniques, culture methods, and phases of bacterial growth. Diagrams are provided to illustrate some concepts.




































































![15. Describe antibiotic sensitivity test (AST) 16. Explain Widal test
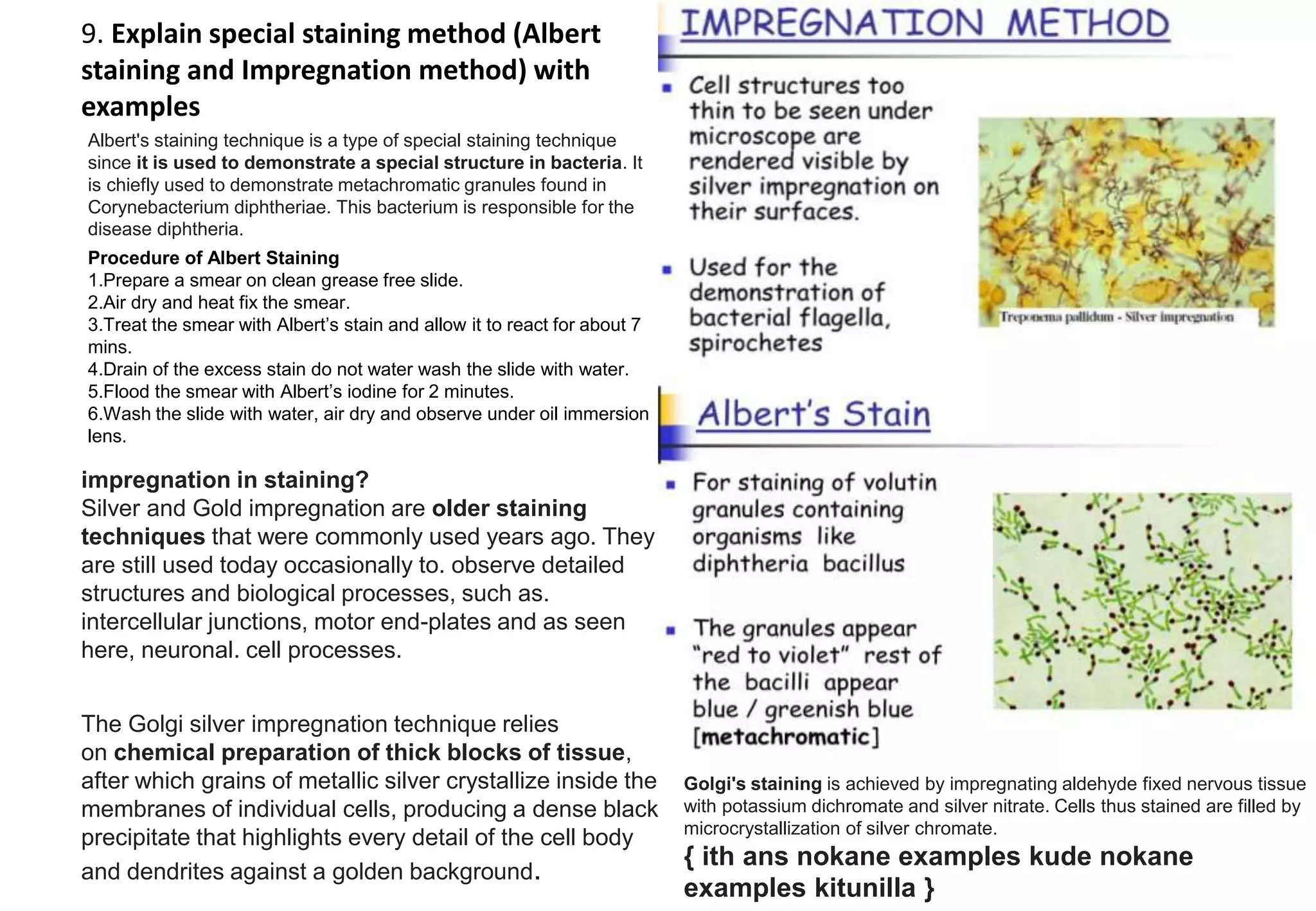
The Widal test measures the capacity of antibodies against LPS
and flagella in the serum of individuals with suspected typhoid
fever to agglutinate cells of S. Typhi; the test was introduced over a
century ago and it is still widely used [20].
What is the normal range of Widal test?
Conclusion: In case of singular Widal test, baseline values for the normal
range was found to be 1:20 - 1:80 for all the antigens (TO, TH, AO, AH, BO,
BH), except BH, for which it was 1:20-1:40.
Widal Test is an agglutination test which detects the presence of
serum agglutinins (H and O) in patients serum with typhoid and
paratyphoid fever
Antibiotic susceptibility testing, or AST, is a widely-used
method of evaluating antibiotic resistance and
determining patient treatment plans in clinical
settings. There are a number of different methods of
AST such as agar dilution, broth dilution and disc
diffusion assays.
What is AST system?
A next-generation phenotyping system is seeking to
revolutionize antibiotic susceptibility testing (AST) in
an effort to begin treating patients faster and to combat
antibiotic resistance.](https://image.slidesharecdn.com/microbiology-1-1-230417120011-ba248e72/75/MICROBIOLOGY-1-1-pptx-72-2048.jpg)







