- Metastatic neck disease is an important prognostic factor in head and neck cancer.
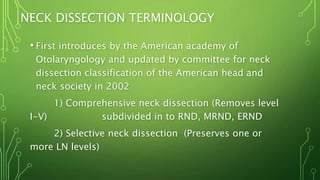
- Management of neck disease involves choices of treatment modality, timing, and combination of treatments which are controversial.
- Assessment of cervical lymphadenopathy involves clinical examination, fine needle aspiration cytology, imaging like ultrasound, CT, MRI, and PET.
- Treatment depends on neck stage - elective neck treatment for N0, neck dissection for N1, neck dissection with postoperative radiation for N2, and debate over treatment for massive N3 nodes.