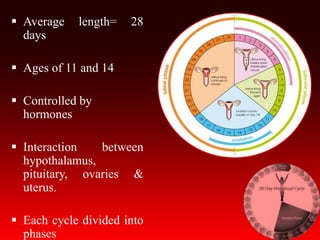
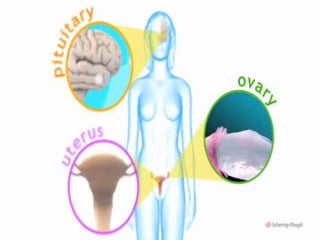
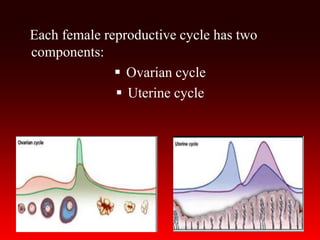
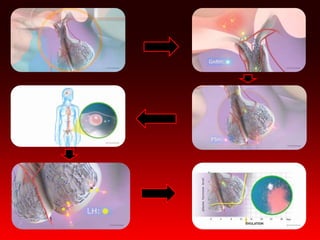
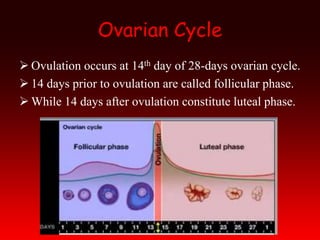
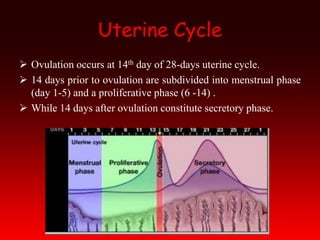
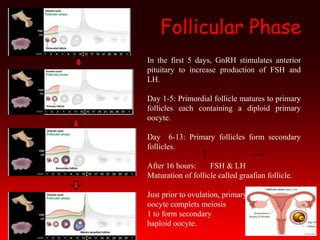
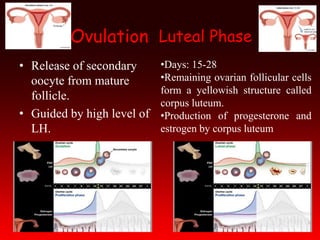
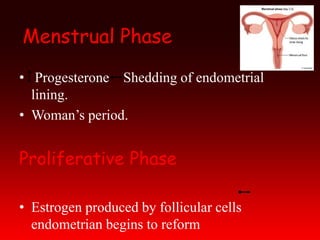
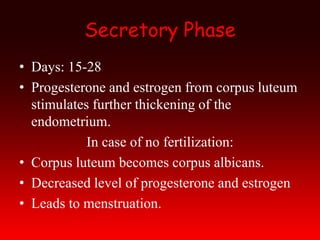
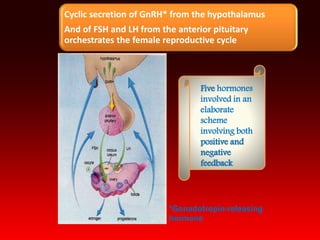
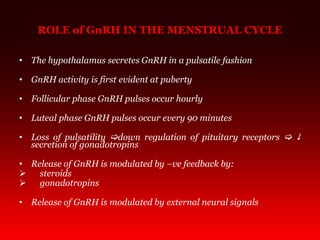
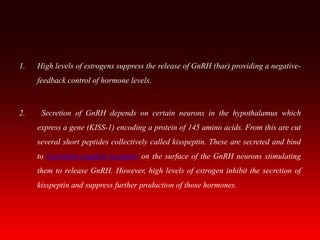
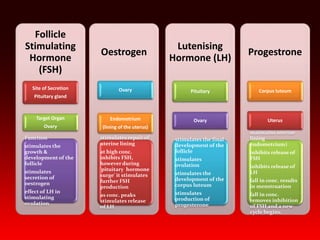
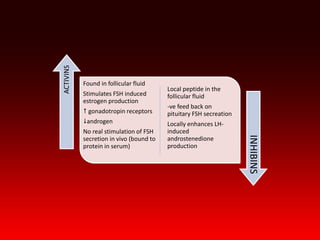
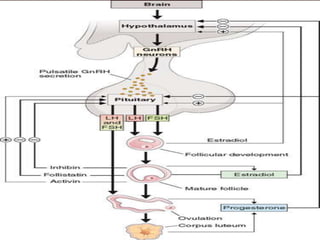
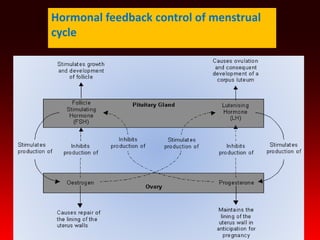
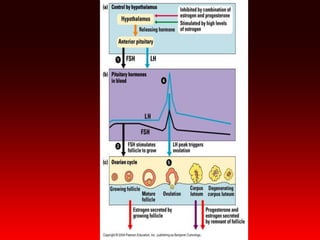
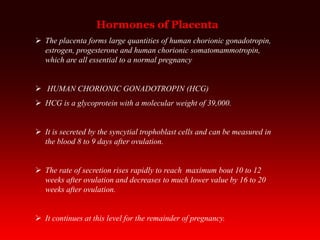
The menstrual cycle is regulated by hormones from the hypothalamus, pituitary gland, and ovaries. It involves both the ovarian cycle and uterine cycle. The ovarian cycle consists of the follicular phase leading up to ovulation on day 14, and the luteal phase after. The uterine cycle involves the menstrual, proliferative, and secretory phases. Hormones like FSH, LH, estrogen, and progesterone are involved in a feedback loop to regulate the cycle. Disorders of the menstrual cycle can cause problems like painful periods or abnormal bleeding.