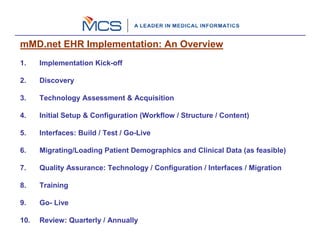
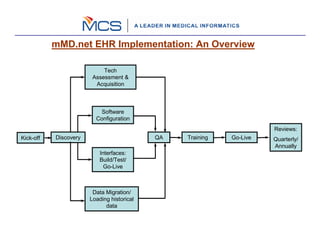
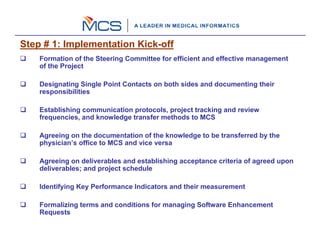
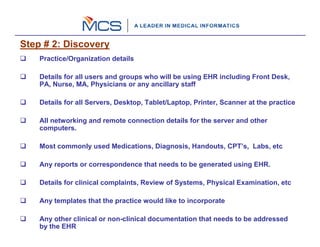
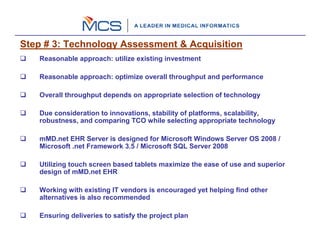
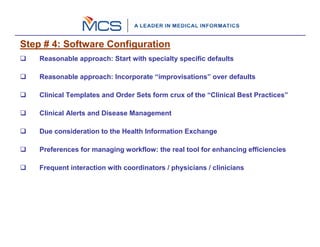
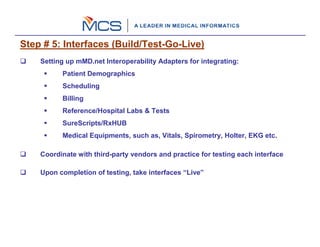
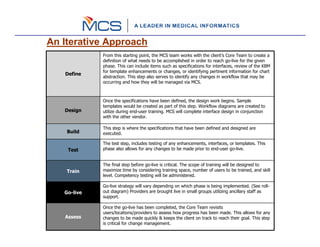
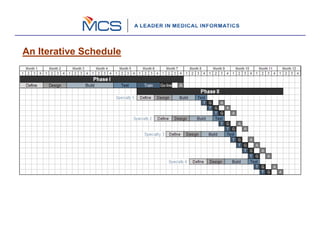
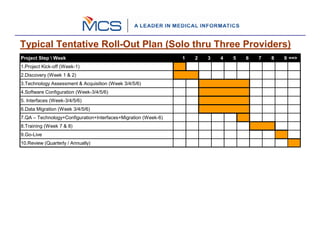
The document outlines a 10 step process for implementing an EHR system called mMD.net. The steps include: 1) implementation kickoff and project planning, 2) assessing needs through discovery, 3) acquiring technology, 4) configuring the software, 5) building and testing interfaces, 6) migrating data, 7) quality assurance testing, 8) training users, 9) going live, and 10) ongoing reviews. The implementation follows an iterative process of defining requirements, designing, building, testing, training, and going live in phases to gradually rollout the EHR system to providers and staff.