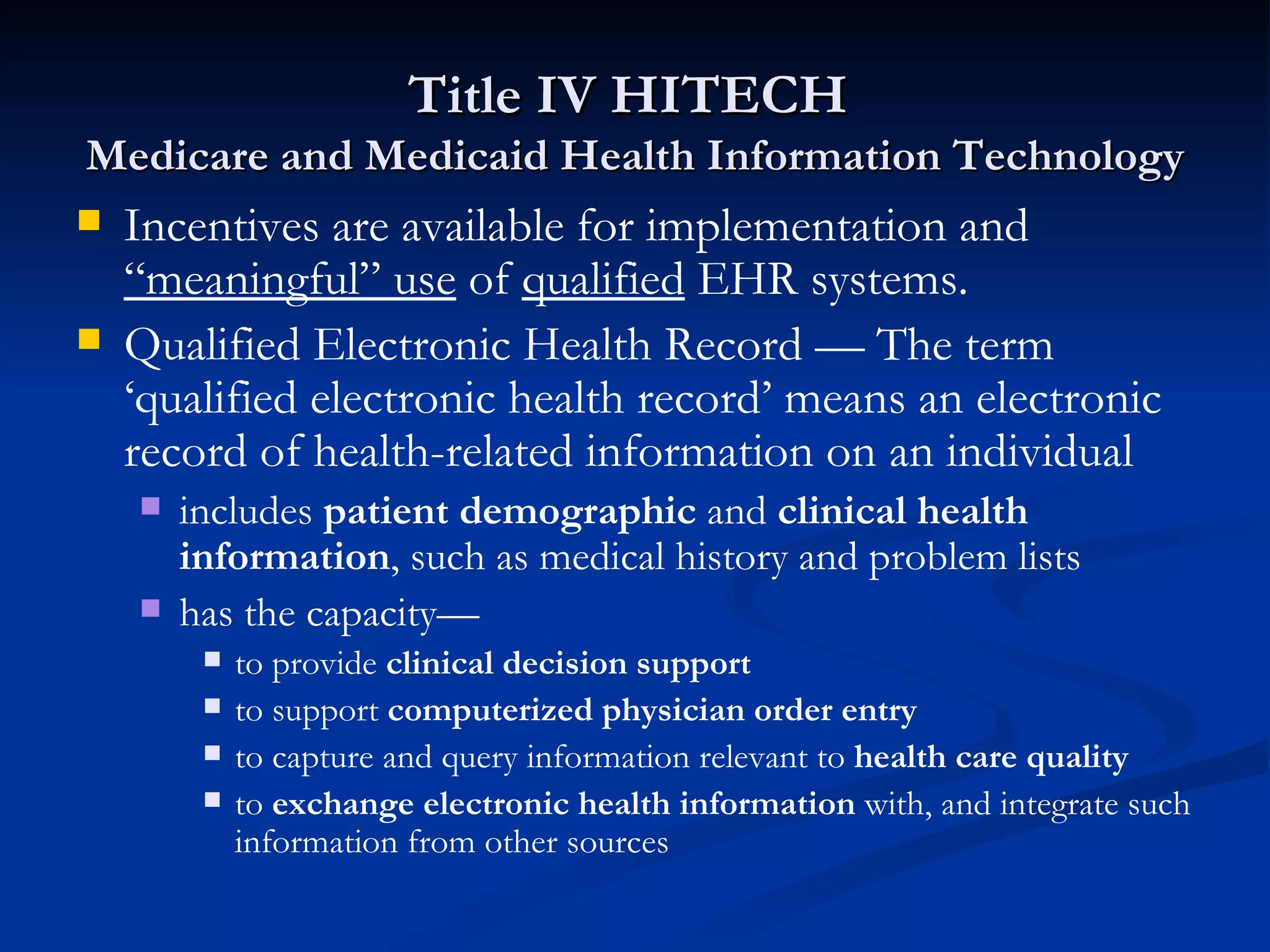
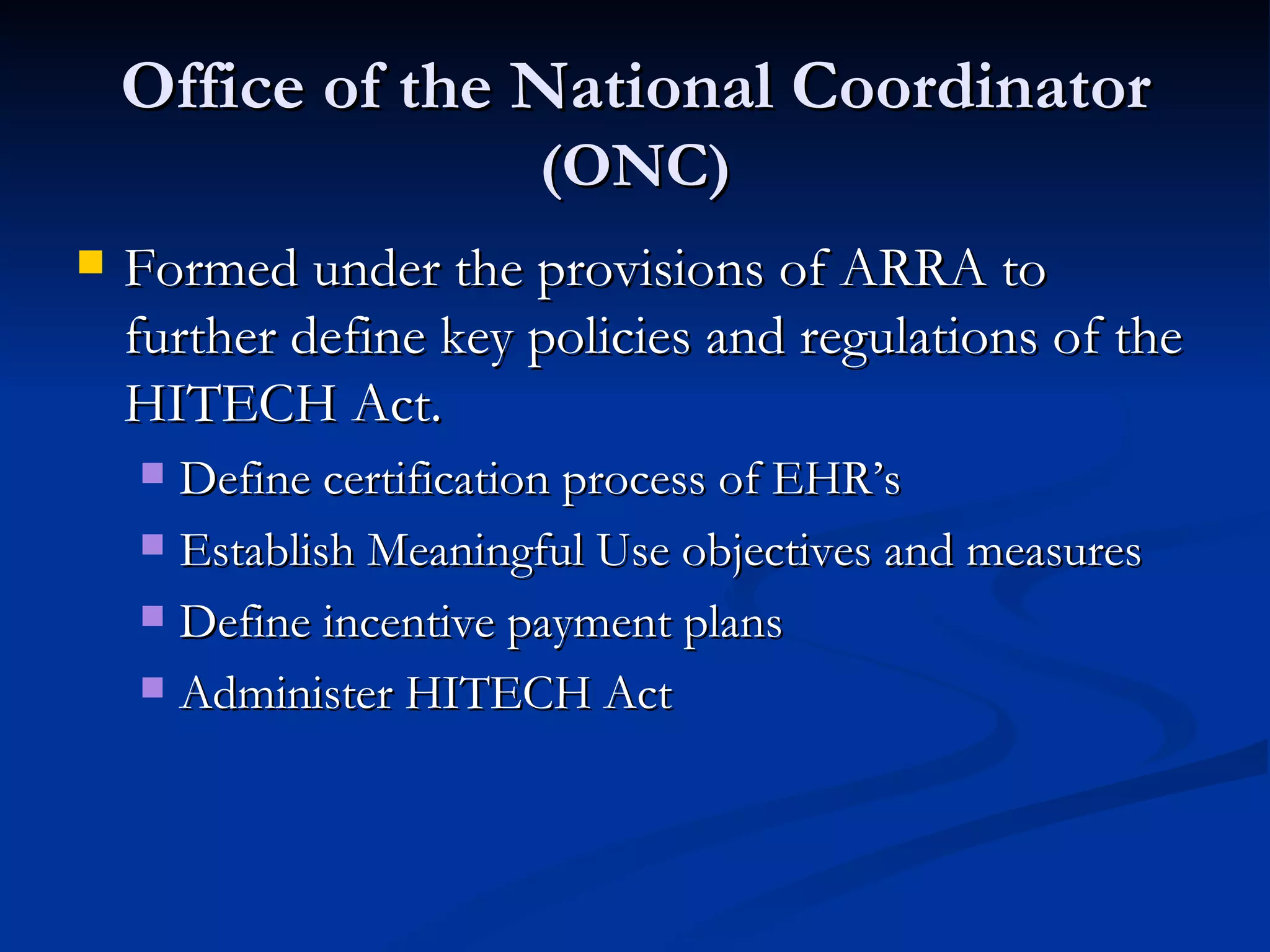
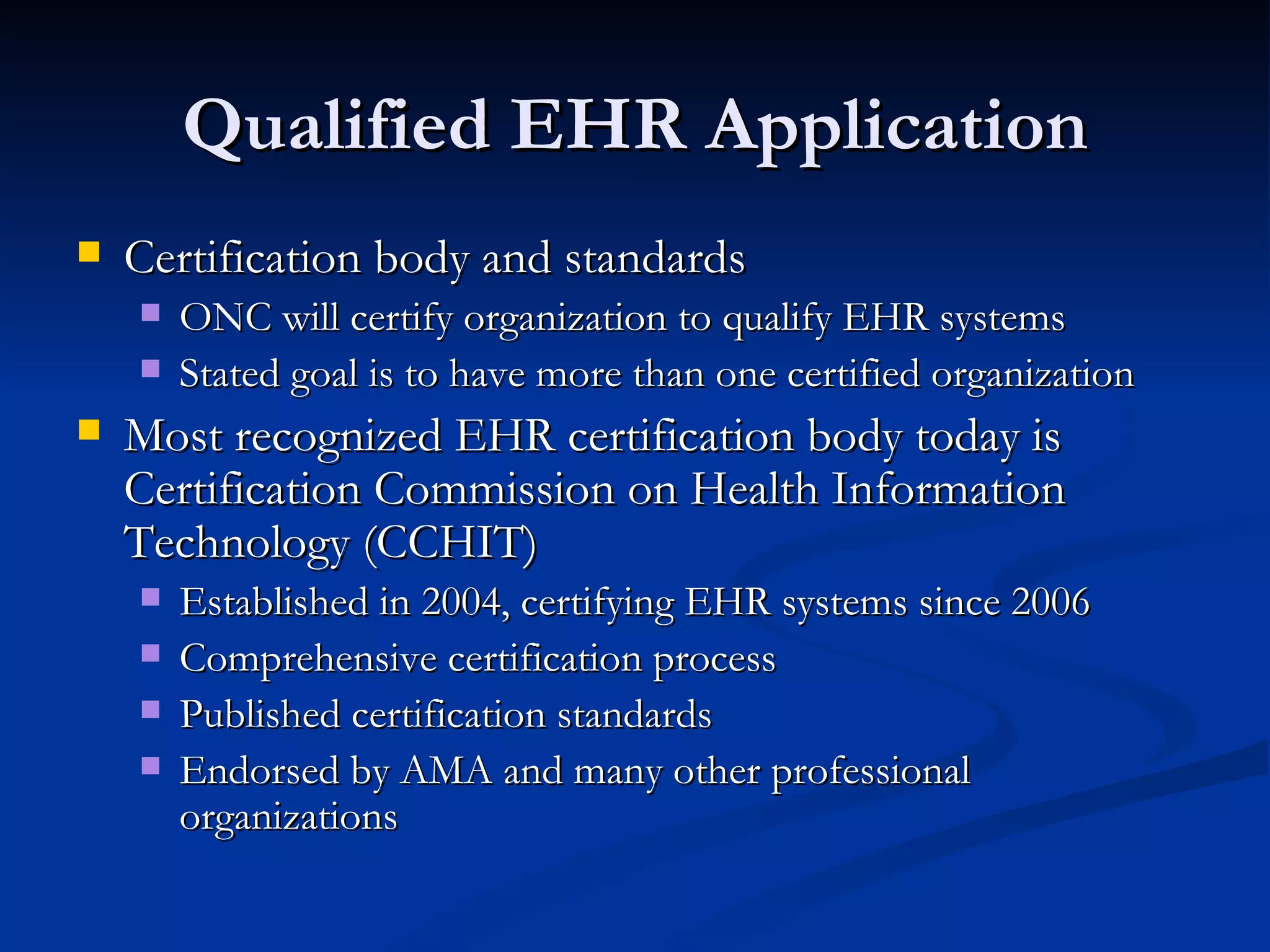
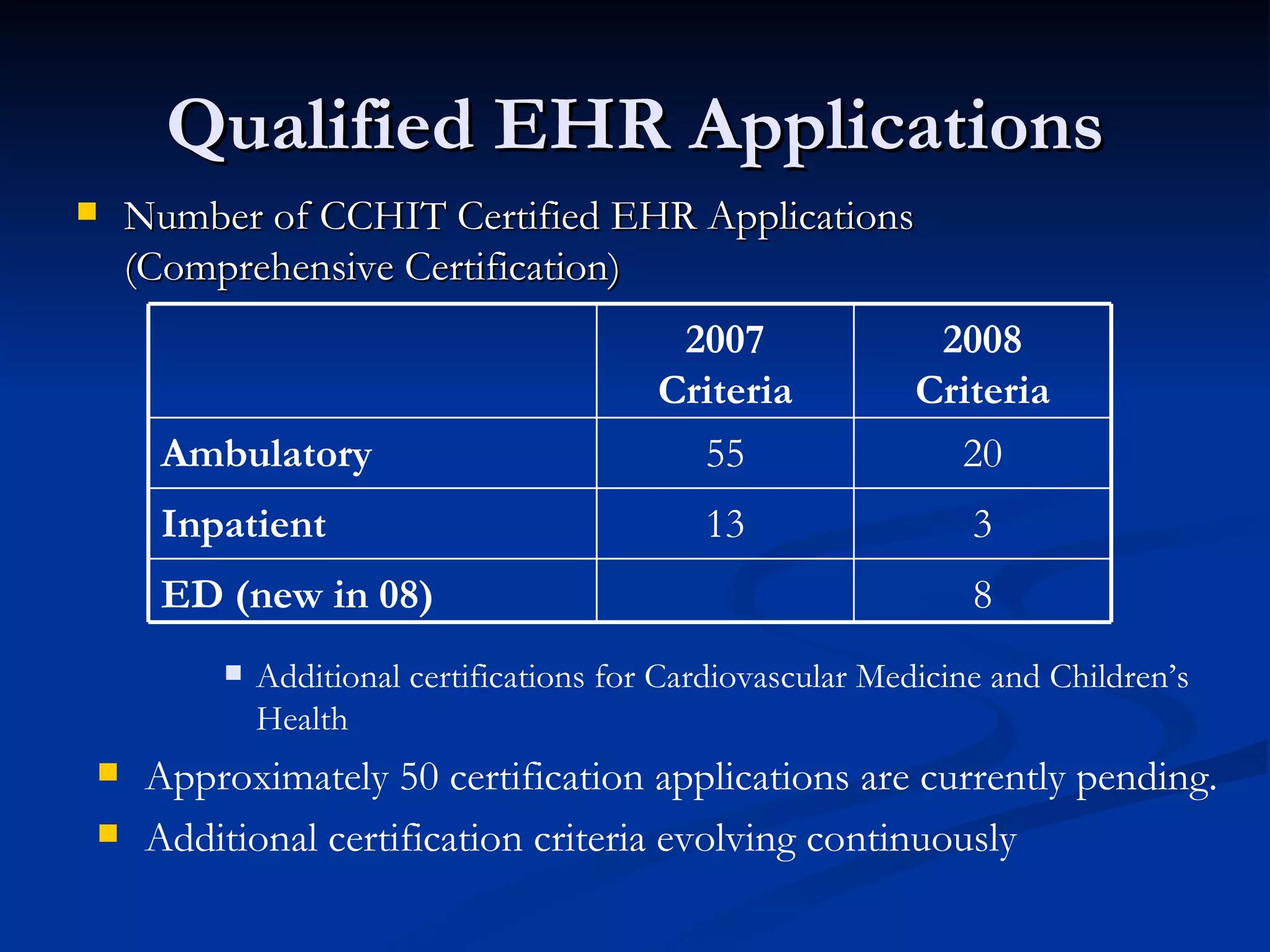
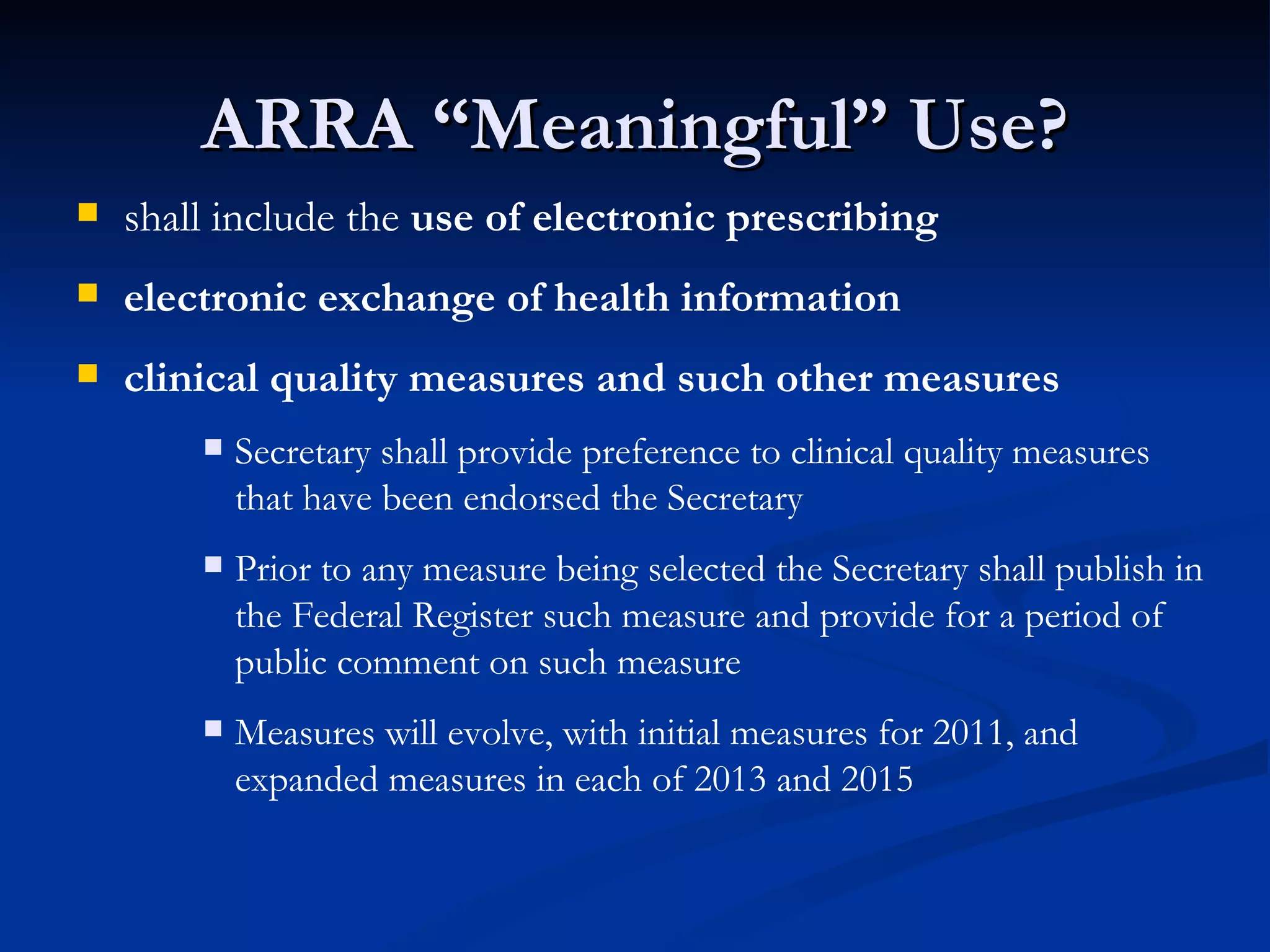
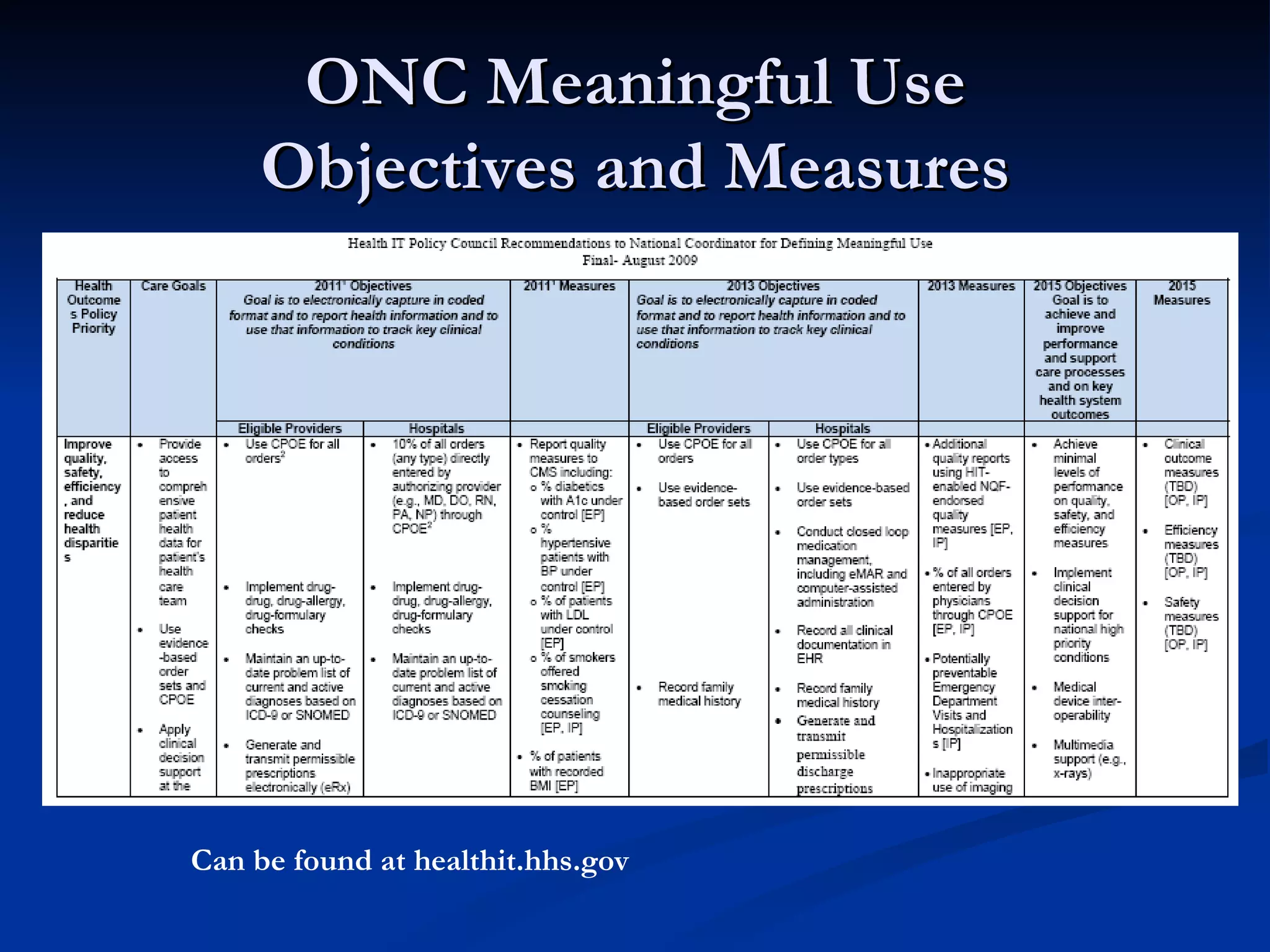
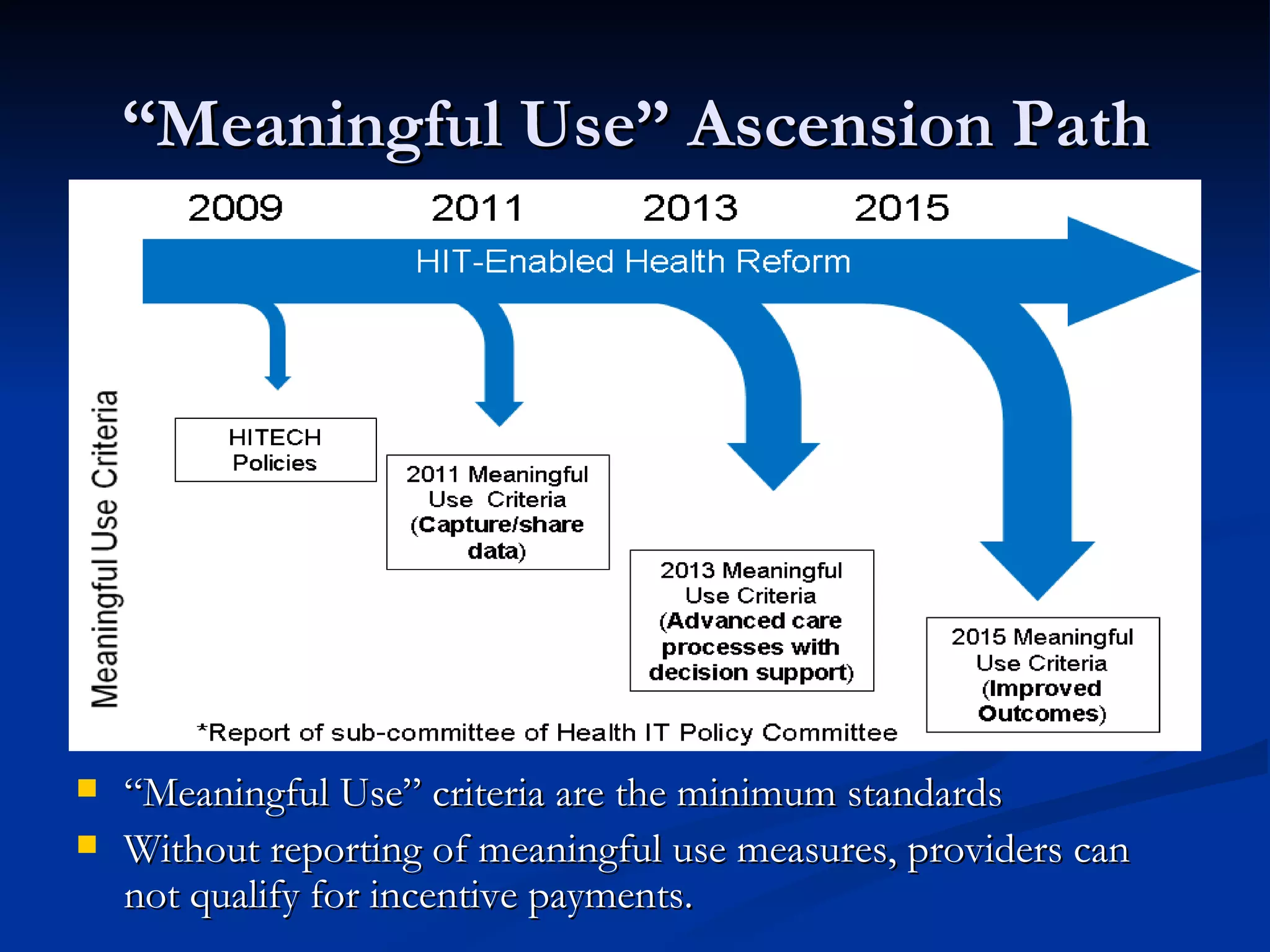
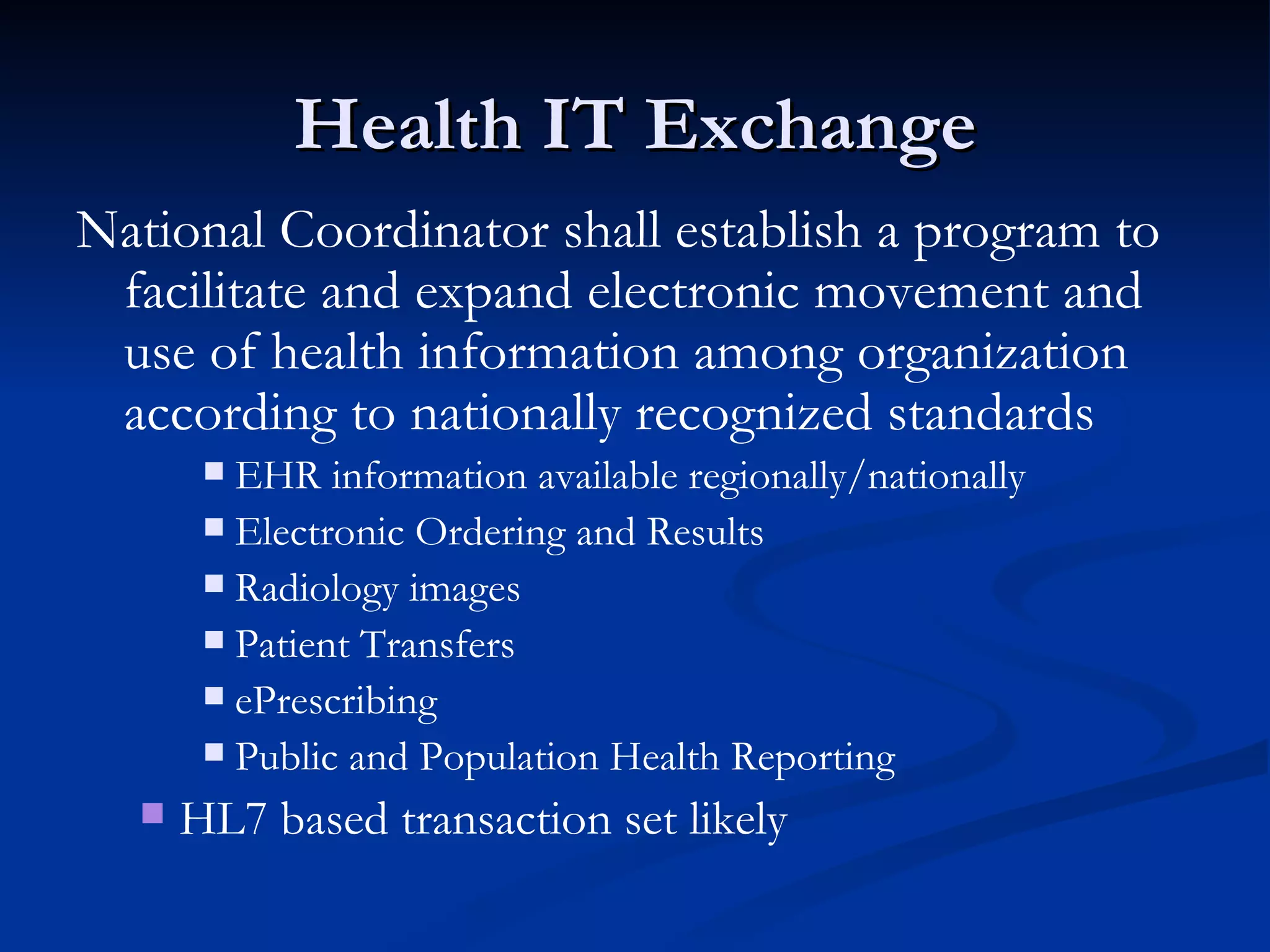
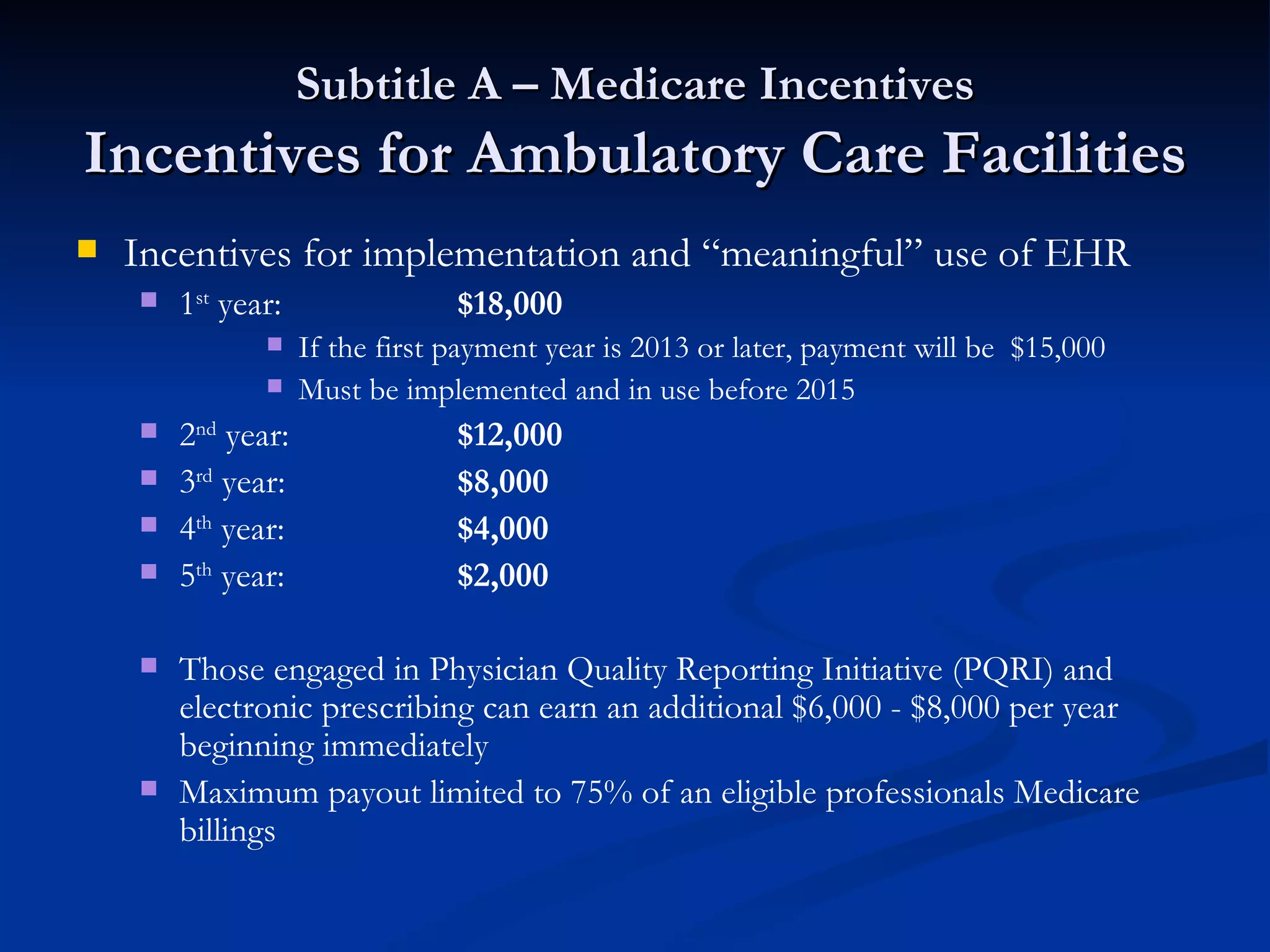
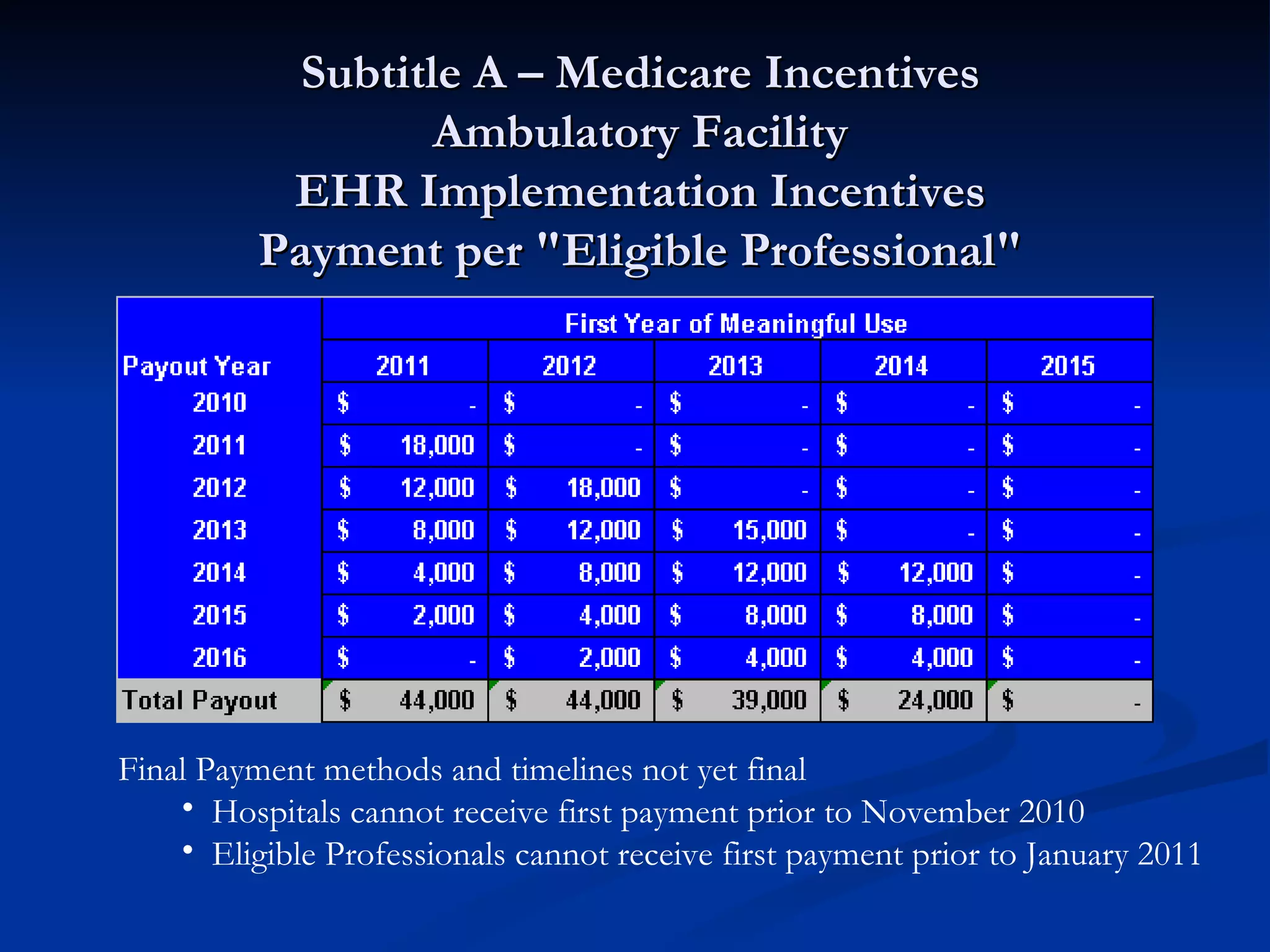
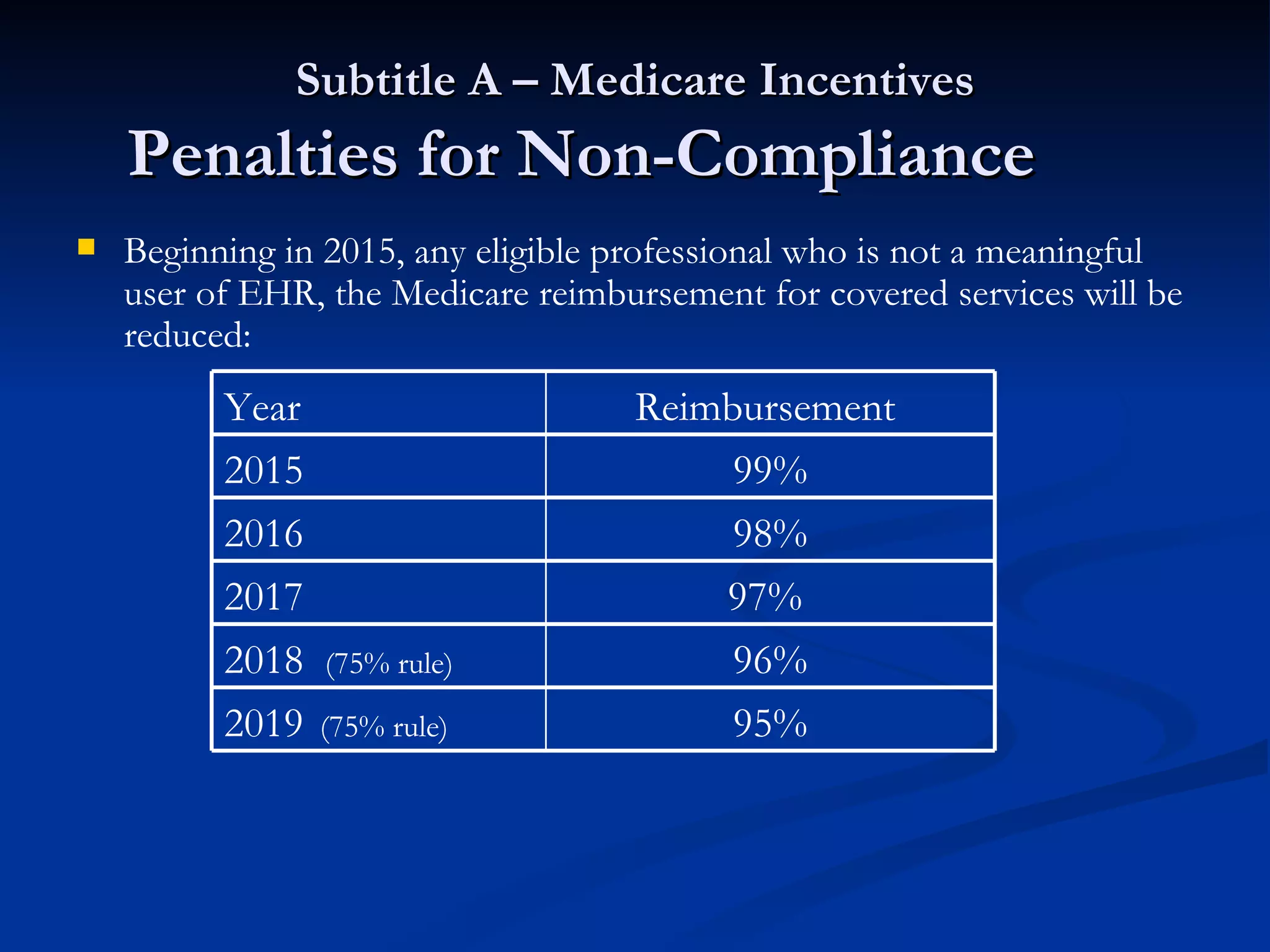
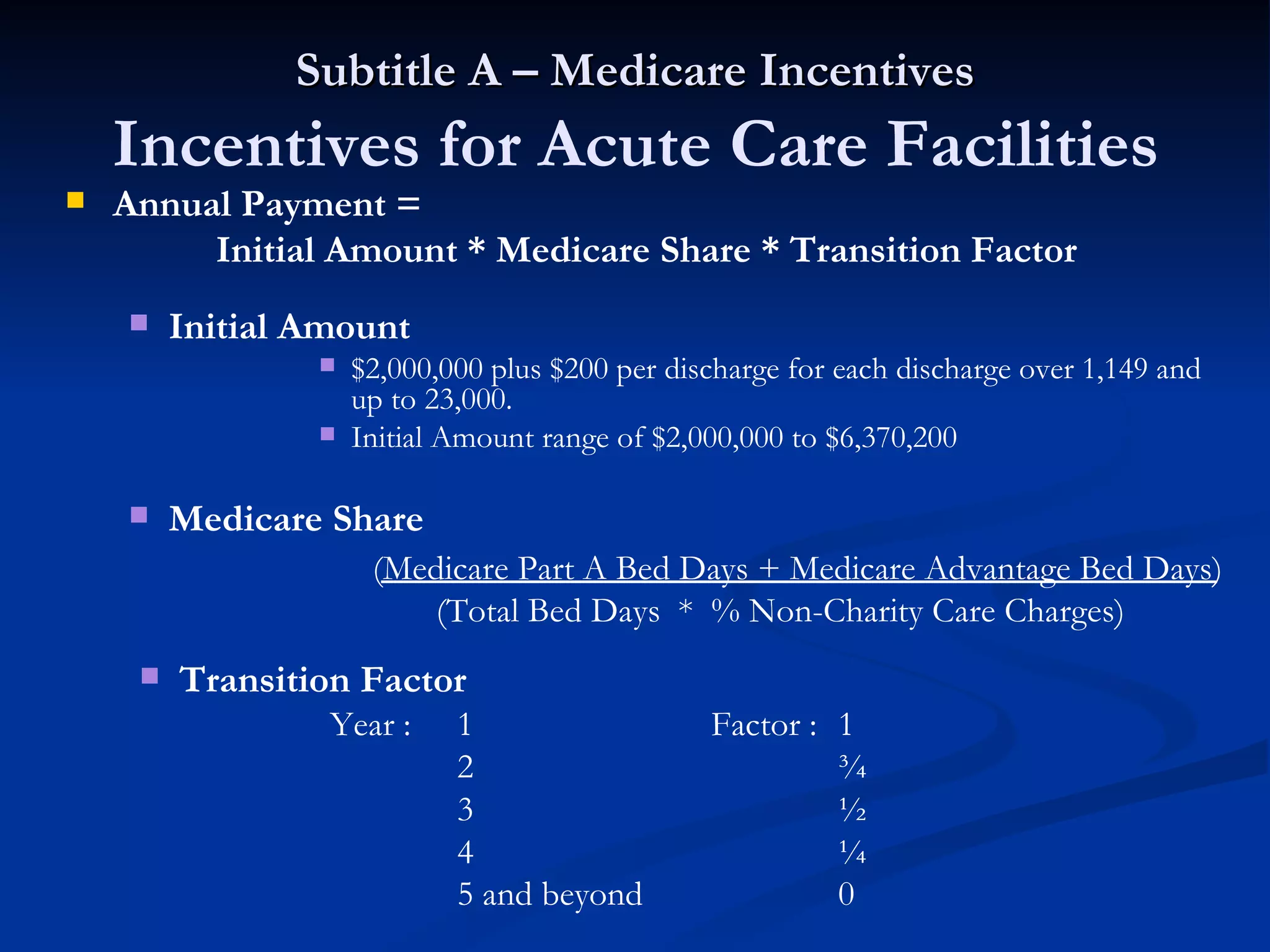
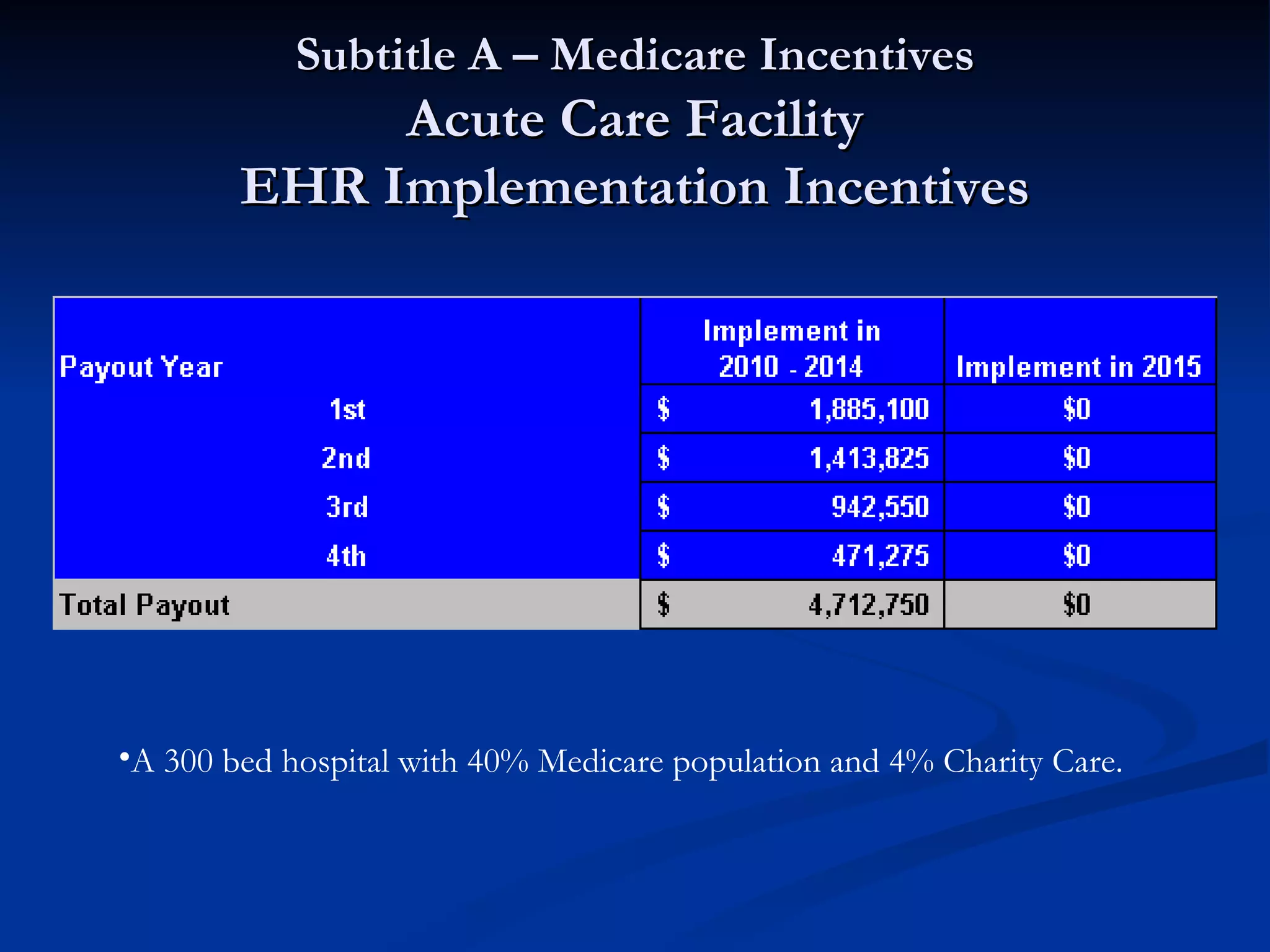
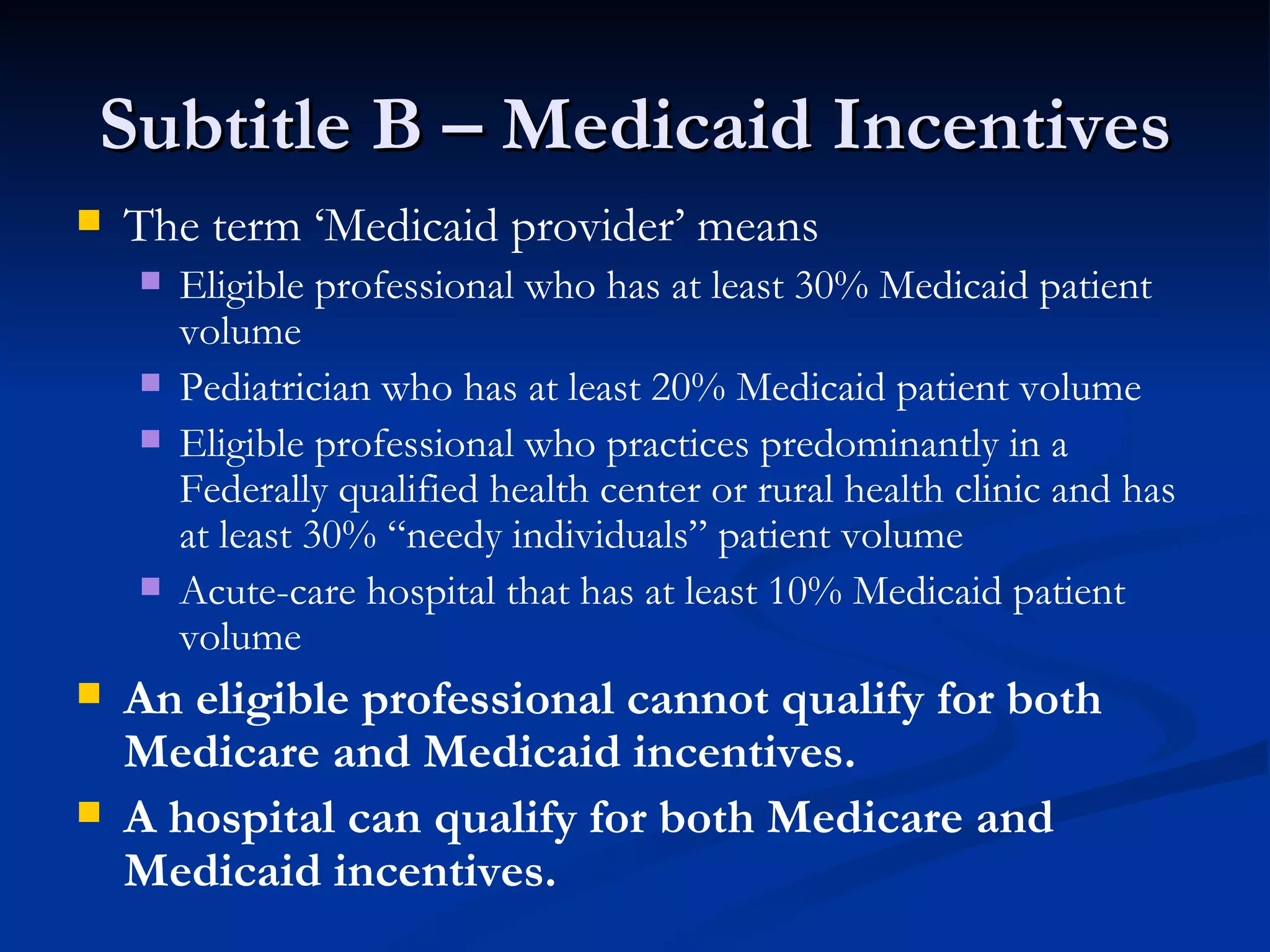
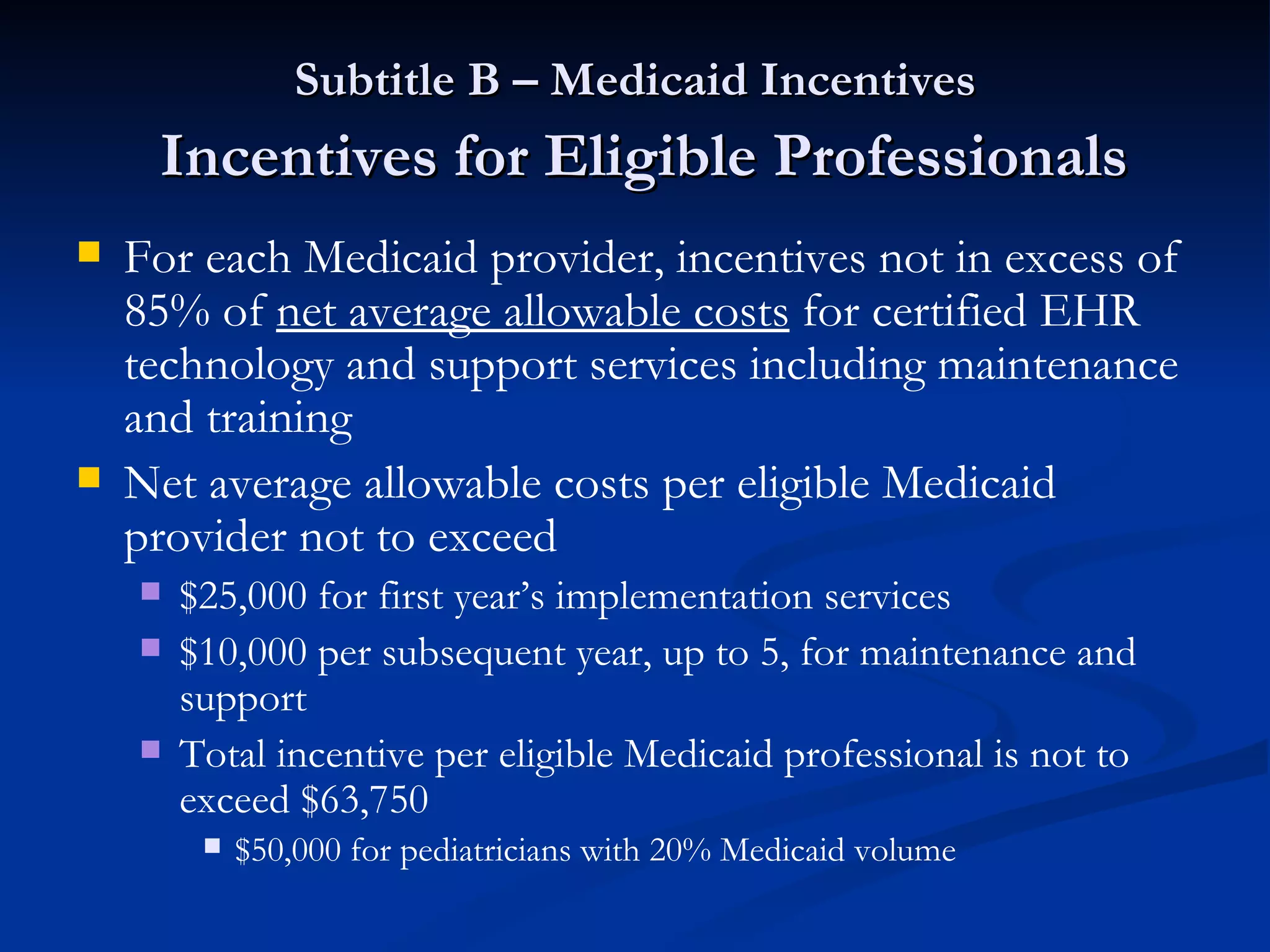
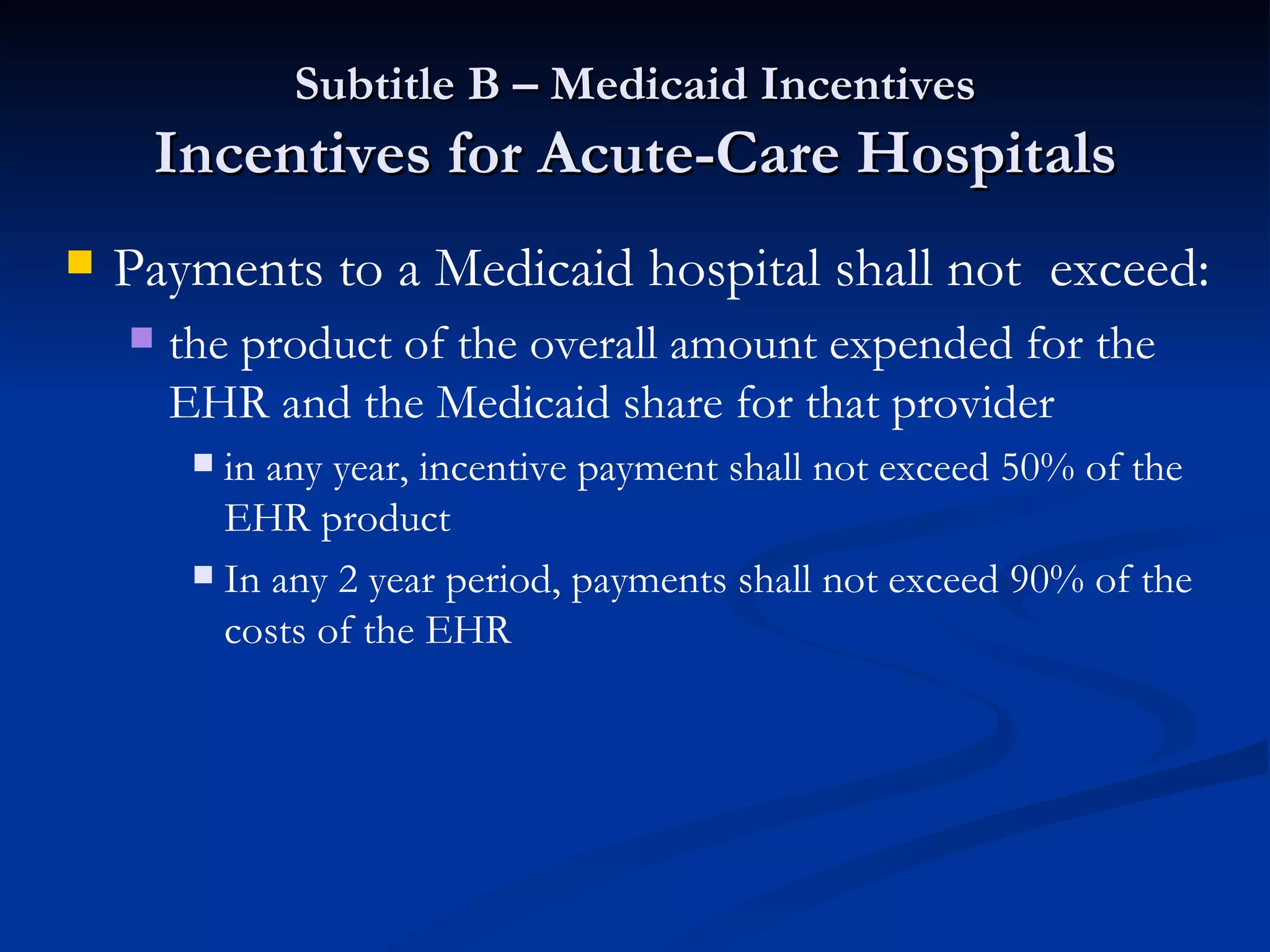
The document summarizes the American Recovery and Reinvestment Act (ARRA) and its impact on electronic health records. It provides incentives for hospitals and physicians to implement qualified electronic health records systems and demonstrate meaningful use by 2015. Those that do not implement EHRs will face penalties after 2015. The ARRA sets standards for qualified EHRs and meaningful use, and provides Medicare and Medicaid incentive payments to support implementation from 2009 to 2015.




![Q & A Dan Falke [email_address] (513) 227-2740 Jeff Burke [email_address] (513) 702-6846](https://image.slidesharecdn.com/circuitehrpresentation-090918121331-phpapp02/75/The-Circuit-EHR-Presentation-34-2048.jpg)