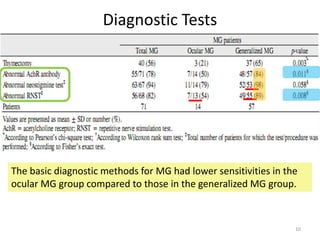
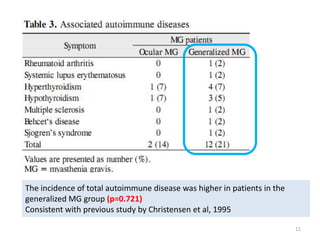
This study compared the clinical manifestations of 71 patients with ocular myasthenia gravis (MG) to those with generalized MG. Patients with generalized MG had a higher rate of other autoimmune diseases and required long-term steroid treatment more often than those with ocular MG alone. Both groups experienced similar ophthalmic symptoms. The study recommends regular eye exams for all MG patients due to risks from autoimmune diseases and long-term steroid use.