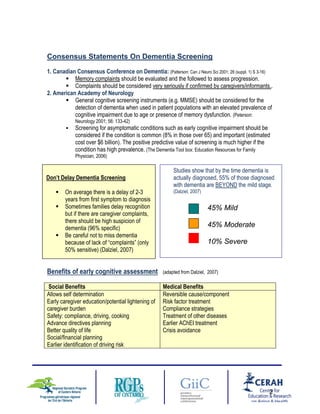
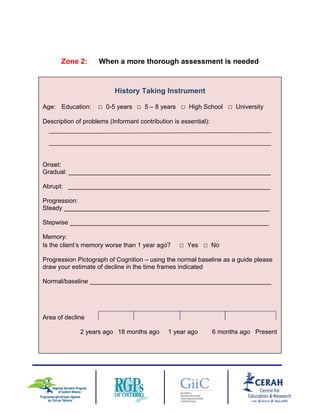
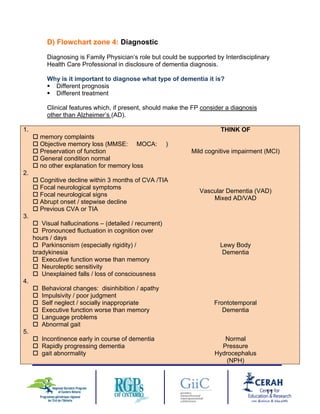
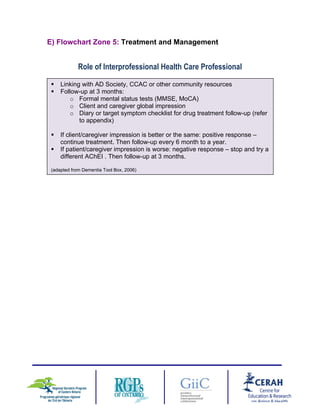
Dementia is a cognitive decline that interferes with daily functioning. It affects memory, language, judgment, and other thinking abilities. Risk increases with age and the presence of vascular risk factors. The prevalence of dementia among those over 65 is 8%, representing a growing challenge. Early screening allows for social and medical benefits like safety planning and earlier treatment. A thorough assessment considers cognitive tests, functional ability, behavioral changes, and input from caregivers to determine if a diagnosis of dementia is appropriate.